Parasympatholytics, also known as anticholinergics or parasympathetic blockers, are a class of drugs that antagonize the effects of acetylcholine (ACh) at muscarinic receptors in the parasympathetic nervous system. These drugs inhibit the parasympathetic nervous system’s actions, leading to various physiological effects.
Classification of Parasympatholytics
Parasympatholytics can be classified based on their chemical structure or their pharmacological effects. Chemically, they include tertiary amines (e.g., atropine, scopolamine) and quaternary ammonium compounds (e.g., ipratropium bromide). Pharmacologically, they can be categorized as antimuscarinic agents, blocking the effects of ACh at muscarinic receptors.
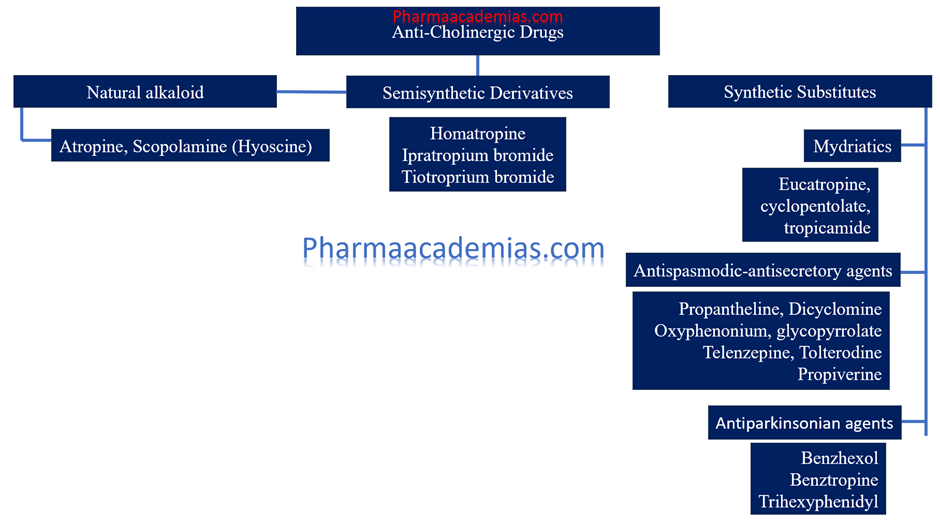
1. Natural alkaloids
Atropine, hyoscine (scopolamine)
2. Semisynthetic derivatives
Homatropine, ipratropium bromide, tiotroprium bromide
3. Synthetic substitutes
• Mydriatics
Eucatropine, cyclopentolate, tropicamide
• Antispasmodic-antisecretory agents
Propantheline, dicyclomine, oxyphenonium, glycopyrrolate, telenzepine, tolterodine, propiverine
• Antiparkinsonian agents
Benzhexol, benztropine, trihexyphenidyl
1. Natural Alkaloids
Natural alkaloids are compounds derived from plants that exhibit anticholinergic properties. They are naturally occurring and are often used in medical treatments for their effects on the nervous system.
Atropine
Atropine is a medication derived from the belladonna plant (Atropa belladonna) and other plants of the nightshade family. It is a tropane alkaloid and functions as an anticholinergic agent, meaning it inhibits the action of the neurotransmitter acetylcholine at muscarinic receptors in the nervous system.
– Source: Atropine is derived from the plant Atropa belladonna (deadly nightshade).
– Uses: It is used to dilate pupils during eye examinations, as an antidote for organophosphate poisoning, and to treat bradycardia (slow heart rate).
– Mechanism of Action: Atropine works by blocking the muscarinic acetylcholine receptors, thereby inhibiting parasympathetic nervous system activity.
Hyoscine (Scopolamine)
Scopolamine, also known as hyoscine, is a medication and a naturally occurring tropane alkaloid drug that is used primarily for the treatment of motion sickness and postoperative nausea and vomiting. It belongs to the antimuscarinic class of medications and works by blocking the action of acetylcholine, a neurotransmitter in the body.
– Source: Hyoscine is derived from plants of the nightshade family, such as Hyoscyamus niger (henbane).
– Uses: It is commonly used to prevent motion sickness and nausea, as well as to reduce secretions in palliative care.
– Mechanism of Action: Like atropine, hyoscine blocks muscarinic receptors, inhibiting parasympathetic nerve impulses.
2. Semisynthetic Derivatives
Semisynthetic derivatives are chemically modified versions of natural alkaloids. These modifications enhance their therapeutic effects or reduce unwanted side effects.
Homatropine
Homatropine is a medication that belongs to the class of anticholinergic drugs. It is derived from atropine and has similar effects but is generally considered to be less potent. Homatropine is primarily used in ophthalmology and sometimes in other medical fields.
– Uses: It is used as an eye drop to dilate pupils for ophthalmic examinations and procedures.
– Mechanism of Action: Homatropine works similarly to atropine but has a shorter duration of action.
Ipratropium Bromide
Ipratropium is another medication in the antimuscarinic class, but it is primarily used as a bronchodilator to treat respiratory conditions such as chronic obstructive pulmonary disease (COPD) and asthma. Unlike other antimuscarinic drugs like scopolamine or glycopyrrolate, which have broader effects on various body parts, ipratropium primarily targets the respiratory system.
Ipratropium works by blocking the action of acetylcholine at muscarinic receptors in the airways, leading to the relaxation of the smooth muscles surrounding the bronchial tubes. This relaxation results in bronchodilation, which helps to relieve symptoms such as wheezing, shortness of breath, and coughing associated with COPD and asthma.
– Uses: It is used as a bronchodilator in the treatment of chronic obstructive pulmonary disease (COPD) and asthma.
– Mechanism of Action: Ipratropium blocks muscarinic receptors in the bronchial smooth muscle, leading to bronchodilation.
Tiotropium Bromide
Tiotropium is a long-acting anticholinergic bronchodilator used to manage chronic obstructive pulmonary disease (COPD) and asthma. It is also prescribed to reduce exacerbations in COPD patients and improve symptoms such as shortness of breath and wheezing.
Tiotropium works by blocking the action of acetylcholine at muscarinic receptors in the airways, leading to bronchodilation and improved airflow. Unlike short-acting anticholinergics, tiotropium has a longer duration of action, allowing for once-daily dosing.
– Uses: Similar to ipratropium, tiotropium is used for long-term management of COPD and asthma.
– Mechanism of Action: Tiotropium has a prolonged duration of action due to its slow dissociation from muscarinic receptors, providing sustained bronchodilation.
3. Synthetic Substitutes
Synthetic substitutes are entirely man-made compounds designed to mimic or improve upon the effects of natural alkaloids. They are often categorized based on their specific therapeutic uses.
Mydriatics: Mydriatics are drugs used to dilate pupils.
– Eucatropine
Eucatropine is a synthetic compound that is classified as an anticholinergic drug. It is mainly used in ophthalmology, much like other anticholinergics, to induce mydriasis (pupil dilation) and cycloplegia (paralysis of the ciliary muscle). Its primary applications are in diagnostic procedures and treatments requiring pupil dilation and ciliary muscle paralysis.
– Uses: Used in ophthalmic procedures to dilate the pupils.
– Mechanism of Action: Blocks muscarinic receptors in the eye, causing pupil dilation.
– Cyclopentolate
Cyclopentolate is an anticholinergic medication used primarily in ophthalmology. It is employed to dilate the pupils (mydriasis) and paralyze the ciliary muscle (cycloplegia) for diagnostic and therapeutic purposes.
– Uses: Employed in eye exams to achieve pupil dilation.
– Mechanism of Action: Inhibits muscarinic receptors, leading to temporary paralysis of the ciliary muscle and dilation of the pupil.
– Tropicamide
Tropicamide is a medication primarily used as a mydriatic agent to dilate the pupil of the eye for diagnostic and therapeutic purposes. It belongs to the class of drugs known as anticholinergic agents, specifically muscarinic receptor antagonists.
When applied to the eye, tropicamide works by blocking the action of acetylcholine at the muscarinic receptors in the iris sphincter muscle and ciliary muscle. By inhibiting these receptors, tropicamide causes relaxation of the iris sphincter muscle, leading to pupil dilation (mydriasis), and paralysis of the ciliary muscle, resulting in cycloplegia (loss of accommodation).
– Uses: Commonly used for pupil dilation in eye exams.
– Mechanism of Action: Acts on muscarinic receptors to cause pupil dilation with a short duration of action.
Antispasmodic-Antisecretory Agents
These agents are used to reduce muscle spasms and secretions.
– Propantheline
Propantheline is an anticholinergic medication that belongs to a class of drugs known as antimuscarinics or antispasmodics. It is used to reduce the effects of acetylcholine in the body, thereby decreasing spasms and secretions in various organs.
– Uses: Treats excessive sweating, stomach cramps, and other spasmodic conditions.
– Mechanism of Action: Blocks acetylcholine receptors to reduce spasms and secretions.
– Dicyclomine
Dicyclomine, also known by its brand name Bentyl among others, is an anticholinergic medication used primarily to treat gastrointestinal conditions that involve spasms, cramps, and discomfort.
– Uses: Used to treat irritable bowel syndrome (IBS).
– Mechanism of Action: Relieves muscle spasms in the gastrointestinal tract by blocking muscarinic receptors.
– Oxyphenonium
Oxyphenonium is another anticholinergic medication, similar to dicyclomine, used primarily to treat gastrointestinal disorders characterized by spasms and cramps.
– Uses: Alleviates gastrointestinal spasms and hypersecretory conditions.
– Mechanism of Action: Inhibits muscarinic receptors to decrease secretions and spasms.
– Glycopyrrolate
Glycopyrrolate is a medication that belongs to the antimuscarinic class, similar to scopolamine and homatropine. It is commonly used to reduce saliva, respiratory secretions, and stomach acid production during surgical procedures, particularly in anesthesia. Glycopyrrolate works by blocking the action of acetylcholine at muscarinic receptors, thereby inhibiting the effects of excessive secretions in various parts of the body.
– Uses: Reduces drooling in children with cerebral palsy and decreases secretions during anesthesia.
– Mechanism of Action: Blocks muscarinic receptors, reducing salivary and respiratory secretions.
– Telenzepine
Telenzepine is a medication that belongs to the class of drugs known as muscarinic receptor antagonists. It is primarily used to treat peptic ulcers and other gastrointestinal conditions.
Like pirenzepine, telenzepine works by selectively blocking the action of acetylcholine at muscarinic receptors in the stomach. By inhibiting gastric acid secretion, telenzepine helps to promote the healing of peptic ulcers and relieve symptoms associated with excessive stomach acid, such as heartburn and indigestion.
– Uses: Treats peptic ulcers by reducing gastric acid secretion.
– Mechanism of Action: Selectively inhibits muscarinic receptors involved in gastric acid production.
– Tolterodine
Tolterodine is a medication primarily used to treat overactive bladder (OAB) and urinary incontinence. It belongs to the class of drugs known as antimuscarinics or anticholinergics, which work by blocking the action of acetylcholine at muscarinic receptors in the bladder muscle, thereby reducing bladder spasms and involuntary contractions.
By inhibiting these contractions, tolterodine helps increase bladder capacity, decrease urinary frequency, and reduce urgency and urinary incontinence episodes. It is commonly prescribed for conditions such as urge incontinence and urgency-frequency syndrome.
– Uses: Manages overactive bladder and urinary incontinence.
– Mechanism of Action: Blocks muscarinic receptors in the bladder, reducing urinary urgency and frequency.
– Propiverine
Propiverine is an anticholinergic medication used primarily to treat symptoms associated with overactive bladder (OAB) and other bladder disorders. It works by blocking the action of acetylcholine at muscarinic receptors in the bladder, which helps to reduce involuntary bladder contractions and control symptoms such as urgency, frequency, and urinary incontinence.
– Uses: Also used for overactive bladder treatment.
– Mechanism of Action: Inhibits muscarinic receptors to decrease bladder contractions.
Antiparkinsonian Agents
Antiparkinsonian agents are medications used primarily in the treatment of Parkinson’s disease, a progressive neurological disorder characterized by symptoms such as tremors, rigidity, bradykinesia (slowness of movement), and postural instability. These medications aim to alleviate symptoms by either replacing or enhancing the action of dopamine, a neurotransmitter that is deficient in Parkinson’s disease.
– Benzhexol (Trihexyphenidyl)
Benzhexol, also known by its generic name trihexyphenidyl, is an anticholinergic medication primarily used in the treatment of Parkinson’s disease and also in the management of certain types of dystonia (a movement disorder characterized by involuntary muscle contractions).
– Uses: Treats tremors and muscle stiffness in Parkinson’s disease.
– Mechanism of Action: Blocks muscarinic receptors in the central nervous system, reducing symptoms of Parkinsonism.
– Benztropine
Benztropine, also known by its trade name Cogentin, is an anticholinergic medication primarily used in the treatment of Parkinson’s disease and drug-induced extrapyramidal symptoms (EPS) caused by antipsychotic medications.
– Uses: Used for Parkinson’s disease and drug-induced extrapyramidal symptoms.
– Mechanism of Action: Inhibits muscarinic receptors in the brain, improving motor function in Parkinson’s patients.
– Trihexyphenidyl
Trihexyphenidyl, also known by its brand name Artane among others, is an anticholinergic medication used primarily in the treatment of Parkinson’s disease and also occasionally in the management of extrapyramidal symptoms (EPS) caused by antipsychotic medications.
– Uses: Manages symptoms of Parkinson’s disease and drug-induced extrapyramidal reactions.
– Mechanism of Action: Similar to benzhexol, it blocks central muscarinic receptors to alleviate Parkinsonian symptoms.
Pharmacological Actions:
1. Smooth Muscle Relaxation: Parasympatholytics cause the relaxation of smooth muscles in various organs, including the gastrointestinal tract, urinary bladder, and bronchi. This effect can be beneficial in conditions such as irritable bowel syndrome (IBS), overactive bladder, and bronchospasm.
2. Cardiovascular Effects: Some parasympatholytics can cause mild to moderate tachycardia by blocking the vagal influence on the heart. This effect is particularly seen with tertiary amines like atropine.
3. Mydriasis: Parasympatholytics cause pupil dilation (mydriasis) by blocking the constriction of the iris sphincter muscle mediated by the parasympathetic nervous system. This effect is utilized in ophthalmic examinations and surgeries.
4. Reduction of Glandular Secretions: Parasympatholytics inhibit glandular secretions in various organs, including salivary glands, sweat glands, and mucous glands in the respiratory tract. This action can be beneficial in reducing excessive secretions in conditions like excessive sweating (hyperhidrosis) or respiratory conditions involving excessive bronchial secretions.
5. CNS Effects: Some parasympatholytics have central nervous system effects, including sedation and antiemetic properties. Scopolamine, for example, is used to prevent motion sickness and postoperative nausea and vomiting.
6. Antispasmodic Effects: Parasympatholytics can relieve smooth muscle spasms in gastrointestinal colic and urinary tract spasms.
Indications:
1. Preoperative Medication: Parasympatholytics like scopolamine reduce salivary and respiratory secretions, prevent bradycardia, and decrease gastrointestinal motility before surgery.
2. Ophthalmic Use: Parasympatholytics such as tropicamide and cyclopentolate dilate the pupil for eye examinations and procedures.
3. Gastrointestinal Disorders: Parasympatholytics like hyoscyamine relieve symptoms of irritable bowel syndrome (IBS) and reduce gastrointestinal spasms.
4. Respiratory Disorders: Agents like ipratropium bromide are bronchodilators in chronic obstructive pulmonary disease (COPD) and asthma.
5. Motion Sickness: Scopolamine prevents motion sickness due to its central antimuscarinic effects.
6. Overactive Bladder: Anticholinergic medications such as oxybutynin and tolterodine are used to treat symptoms of overactive bladder by reducing detrusor muscle contractions.
Contraindications:
1. Narrow-Angle Glaucoma: Parasympatholytics can exacerbate narrow-angle glaucoma due to their ability to dilate the pupil, leading to increased intraocular pressure.
2. Urinary Retention: The use of parasympatholytics is contraindicated in patients with urinary retention, as they can further obstruct urinary flow.
3. Gastrointestinal Obstruction: Parasympatholytics may worsen symptoms in patients with gastrointestinal obstruction due to their potential to reduce gastrointestinal motility.
4. Cardiovascular Disease: Tertiary amines like atropine should be used cautiously in patients with cardiovascular disease, as they can cause tachycardia and exacerbate certain cardiac conditions.
5. Pregnancy and Lactation: The use of parasympatholytics during pregnancy and lactation should be avoided unless the potential benefits outweigh the risks, as they can cross the placenta and be excreted in breast milk.
Mechanism of Action of Parasympatholytics
Parasympatholytics competitively antagonize the action of ACh at muscarinic receptors in various tissues throughout the body. By binding to these receptors, parasympatholytics prevent ACh from exerting its effects, inhibiting parasympathetic activity. This blockade results in various physiological responses, including smooth muscle relaxation, glandular secretions inhibition, and increased heart rate.
Pharmacological Actions of Parasympatholytics
1. Smooth Muscle Relaxation: Parasympatholytics cause the relaxation of smooth muscles in various organs, including the gastrointestinal tract, urinary bladder, and bronchi. This effect can be beneficial in conditions such as irritable bowel syndrome (IBS), overactive bladder, and bronchospasm.
2. Cardiovascular Effects: Some parasympatholytics can cause mild to moderate tachycardia by blocking the vagal influence on the heart. This effect is particularly seen with tertiary amines like atropine.
3. Mydriasis: Parasympatholytics cause pupil dilation (mydriasis) by blocking the constriction of the iris sphincter muscle mediated by the parasympathetic nervous system. This effect is utilized in ophthalmic examinations and surgeries.
4. Reduction of Glandular Secretions: Parasympatholytics inhibit glandular secretions in various organs, including salivary glands, sweat glands, and mucous glands in the respiratory tract. This action can be beneficial in reducing excessive secretions in conditions like excessive sweating (hyperhidrosis) or respiratory conditions involving excessive bronchial secretions.
5. CNS Effects: Some parasympatholytics have central nervous system effects, including sedation and antiemetic properties. Scopolamine, for example, is used to prevent motion sickness and postoperative nausea and vomiting.
6. Antispasmodic Effects: Parasympatholytics can relieve smooth muscle spasms in gastrointestinal colic and urinary tract spasms.
Indications of Parasympatholytics
1. Preoperative Medication: Parasympatholytics like scopolamine reduce salivary and respiratory secretions, prevent bradycardia, and decrease gastrointestinal motility before surgery.
2. Ophthalmic Use: Parasympatholytics such as tropicamide and cyclopentolate dilate the pupil for eye examinations and procedures.
3. Gastrointestinal Disorders: Parasympatholytics like hyoscyamine relieve symptoms of irritable bowel syndrome (IBS) and reduce gastrointestinal spasms.
4. Respiratory Disorders: Agents like ipratropium bromide are bronchodilators in chronic obstructive pulmonary disease (COPD) and asthma.
5. Motion Sickness: Scopolamine prevents motion sickness due to its central antimuscarinic effects.
6. Overactive Bladder: Anticholinergic medications such as oxybutynin and tolterodine are used to treat symptoms of overactive bladder by reducing detrusor muscle contractions.
Contraindications of Parasympatholytics
1. Narrow-Angle Glaucoma: Parasympatholytics can exacerbate narrow-angle glaucoma due to their ability to dilate the pupil, leading to increased intraocular pressure.
2. Urinary Retention: The use of parasympatholytics is contraindicated in patients with urinary retention, as they can further obstruct urinary flow.
3. Gastrointestinal Obstruction: Parasympatholytics may worsen symptoms in patients with gastrointestinal obstruction due to their potential to reduce gastrointestinal motility.
4. Cardiovascular Disease: Tertiary amines like atropine should be used cautiously in patients with cardiovascular disease, as they can cause tachycardia and exacerbate certain cardiac conditions.
5. Pregnancy and Lactation: The use of parasympatholytics during pregnancy and lactation should be avoided unless the potential benefits outweigh the risks, as they can cross the placenta and be excreted in breast milk.
In conclusion, parasympatholytics are a diverse class of drugs with a wide range of pharmacological effects. Understanding their mechanism of action, indications, and contraindications is essential for their safe and effective use in clinical practice. These medications are crucial in managing various conditions, including preoperative preparation, ophthalmic procedures, gastrointestinal disorders, and respiratory conditions. However, their use should be carefully considered, and patients should be monitored for potential adverse effects, especially in vulnerable populations.

