Adrenaline (epinephrine) and noradrenaline (norepinephrine) are hormones and neurotransmitters that play essential roles in the body’s response to stress and danger.
1. Adrenaline (Epinephrine):
Adrenaline is a hormone produced by the adrenal glands in response to stress, excitement, or danger. It helps prepare the body for physical exertion or intense situations by increasing heart rate, dilating air passages in the lungs, and mobilizing glucose from energy stores.
2. Noradrenaline (Norepinephrine):
Noradrenaline is both a hormone and a neurotransmitter. It is released from nerve endings in response to stress and acts to increase alertness and arousal, constrict blood vessels to raise blood pressure, and mobilize the body for action.
These hormones are part of the body’s sympathetic nervous system response, commonly known as the “fight or flight” response, which prepares the body to react swiftly to perceived threats or challenges.
Role of Epinephrine/Adrenaline
| Body System | Organ | Receptor Name | Activation/Inhibition | Pharmacological Role | |
| Central Nervous System (CNS) | Brain | Various (indirectly affects other systems) | Activation | Modulates mood, arousal, and alertness; indirectly influences other neurotransmitter systems. | |
| Cardiovascular System | Heart | Beta-1 adrenergic | Activation | Increases heart rate and contractility, enhancing cardiac output. | |
| Blood vessels (skin, kidneys) | Alpha-1 adrenergic | Activation | Causes vasoconstriction in certain vascular beds, increasing blood pressure. | ||
| Blood vessels (skeletal muscles, coronary arteries) | Beta-2 adrenergic | Activation | Causes vasodilation, increasing blood flow to these areas. | ||
| Respiratory System | Lungs | Beta-2 adrenergic | Activation | Causes bronchodilation, making breathing easier during stress. | |
| Metabolic System | Liver, adipose tissue | Alpha-1, Beta-2, Beta-3 adrenergic | Activation | Stimulates glycogenolysis and gluconeogenesis, increasing blood glucose levels; promotes lipolysis. | |
| Digestive System | Gastrointestinal tract | Alpha-2 adrenergic | Activation | Reduces gastrointestinal motility and secretion, conserving energy during stress. | |
| Renal System | Kidneys | Beta-1 adrenergic | Activation | Stimulates renin release, activating the RAAS to increase blood pressure. | |
| Endocrine System | Pancreas, adrenal glands | Alpha-1, Alpha-2, Beta-2 adrenergic | Activation | Modulates insulin and glucagon secretion, affecting blood sugar levels; stimulates ACTH release. | |
| Ocular System | Eyes | Alpha-1 adrenergic | Activation | Causes pupil dilation (mydriasis), improving vision under stress. | |
| Skeletal Muscle | Skeletal muscles | Beta-2 adrenergic | Activation | Increases blood flow to skeletal muscles, enhancing oxygen and nutrient delivery. | |
Role of Norepinephrine/Noradrenaline
| Body System | Organ | Receptor Name | Activation/Inhibition | Pharmacological Role |
| Central Nervous System (CNS) | Brain | Various (indirectly affects other systems) | Activation | Modulates arousal, attention, and mood; indirectly influences other neurotransmitter systems. |
| Cardiovascular System | Heart | Beta-1 adrenergic | Activation | Increases heart rate and contractility, enhancing cardiac output. |
| Blood vessels | Alpha-1 adrenergic | Activation | Causes vasoconstriction, increasing blood pressure. | |
| Respiratory System | Lungs | Beta-2 adrenergic | Activation | Causes mild bronchodilation, aiding breathing during stress. |
| Metabolic System | Liver, adipose tissue | Alpha-1, Beta-2, Beta-3 adrenergic | Activation | Stimulates glycogenolysis and gluconeogenesis, increasing blood glucose levels; promotes lipolysis. |
| Digestive System | Gastrointestinal tract | Alpha-2 adrenergic | Activation | Reduces gastrointestinal motility and secretion, conserving energy during stress. |
| Renal System | Kidneys | Beta-1 adrenergic | Activation | Stimulates renin release, activating the RAAS to increase blood pressure. |
| Endocrine System | Pancreas, adrenal glands | Alpha-1, Alpha-2, Beta-2 adrenergic | Activation | Modulates insulin and glucagon secretion, affecting blood sugar levels. |
| Ocular System | Eyes | Alpha-1 adrenergic | Activation | Causes pupil dilation (mydriasis), improving vision under stress. |
| Skeletal Muscle | Skeletal muscles | Beta-2 adrenergic | Activation | Redistributes blood flow, enhancing oxygen and nutrient delivery to muscles. |
Definition of Sympathomimetics
Sympathomimetics, also known as adrenergic agonists or adrenergic drugs, are a class of medications that mimic the effects of the sympathetic nervous system’s neurotransmitters, particularly norepinephrine and epinephrine. These drugs primarily act on adrenergic receptors, exerting effects similar to those of the sympathetic nervous system.
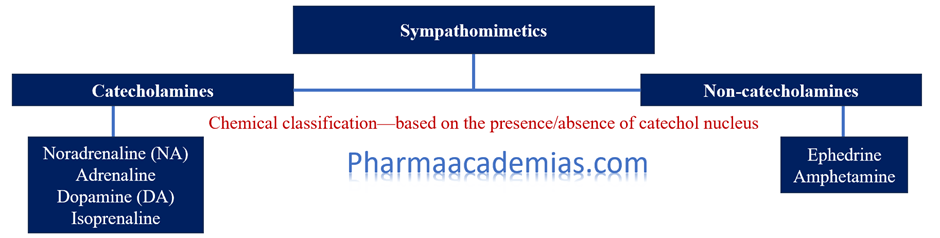
Classification of Sympathomimetics
Sympathomimetics can be classified based on their selectivity to adrenergic receptors, chemical structure, and pharmacological properties. The major classes include:
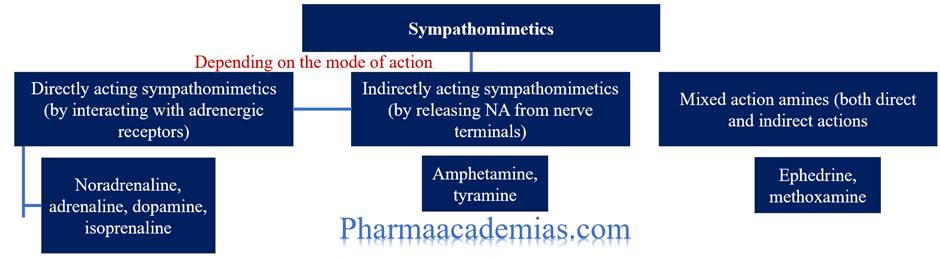
Classification of sympathomimetic drugs based on their mechanism of action:
1. Direct-Acting Agonists
Direct-acting sympathomimetics directly bind to and activate adrenergic receptors on target cells, mimicking the effects of endogenous catecholamines like norepinephrine and epinephrine.
Alpha-adrenergic Agonists:
– Phenylephrine: Phenylephrine is a sympathomimetic drug that acts primarily as an alpha-adrenergic agonist. It is used therapeutically to induce vasoconstriction, primarily targeting alpha-1 adrenergic receptors in the body. This effect leads to an increase in peripheral vascular resistance, resulting in elevated blood pressure and reduced nasal congestion when administered intranasally. Phenylephrine is commonly utilized in the treatment of hypotension, nasal congestion, and as a mydriatic agent in ophthalmology.
– Methoxamine: Methoxamine is another sympathomimetic drug that functions as an alpha-adrenergic agonist. It primarily acts on alpha-1 adrenergic receptors, leading to peripheral vasoconstriction and an increase in blood pressure. This medication is used clinically to treat hypotension, particularly in situations where maintaining adequate blood pressure is crucial, such as during anesthesia or shock. Methoxamine is administered intravenously and can cause side effects such as hypertension, reflex bradycardia, and headache.
Beta-adrenergic Agonists:
– Isoproterenol: Isoproterenol, also known as isoprenaline, is a synthetic sympathomimetic amine that acts as a non-selective beta-adrenergic receptor agonist. It mimics the actions of naturally occurring catecholamines like adrenaline (epinephrine).
Mechanism of Action: Isoproterenol stimulates beta-adrenergic receptors, primarily targeting both beta-1 and beta-2 receptors.
Beta-1 receptors: Located primarily in the heart, stimulation increases heart rate (chronotropy), contractility (inotropy), and conduction velocity (dromotropy).
Beta-2 receptors: Found in smooth muscle of bronchioles and blood vessels, stimulation leads to bronchodilation and vasodilation.
– Salbutamol (Albuterol): Salbutamol, also known as albuterol, is a widely used sympathomimetic medication primarily known for its selective beta-2 adrenergic agonist properties.
Mechanism of Action: Salbutamol selectively stimulates beta-2 adrenergic receptors, which are predominantly found in the smooth muscle of the bronchioles (airways) and to a lesser extent in blood vessels.
Bronchodilation: Activation of beta-2 receptors causes relaxation of bronchial smooth muscle, leading to widening of the airways and relief of bronchospasm.
Vasodilation: Salbutamol can also cause vasodilation in peripheral blood vessels, which may lead to a decrease in peripheral vascular resistance and a mild increase in heart rate (beta-1 receptor effect).
2. Indirect-Acting Agonists
Indirect-acting sympathomimetics enhance the release of endogenous catecholamines (norepinephrine and dopamine) from nerve terminals or inhibit their reuptake from the synaptic cleft.
Release Stimulants:
– Amphetamine: Increases the release of norepinephrine and dopamine from presynaptic nerve terminals. It has stimulant effects and is used in attention deficit hyperactivity disorder (ADHD) and narcolepsy.
Mechanism of Action: Amphetamine acts primarily by increasing the release and blocking the reuptake of the neurotransmitters dopamine, norepinephrine, and serotonin in the brain. This leads to increased synaptic concentrations of these neurotransmitters, enhancing their effects on the central nervous system.
– Ephedrine: Acts similarly to amphetamine but also has direct alpha and beta-adrenergic receptor agonist effects. It is used for its bronchodilator and stimulant properties.
Mechanism of Action:
Direct Action: Ephedrine acts directly on alpha and beta-adrenergic receptors, stimulating them similarly to endogenous catecholamines like adrenaline (epinephrine). This direct stimulation leads to effects such as increased heart rate, bronchodilation, and vasoconstriction.
Indirect Action: Ephedrine also increases the release of norepinephrine from nerve terminals, prolonging its action in the body.
Reuptake Inhibitors:
– Cocaine: Inhibits the reuptake of norepinephrine and dopamine from the synaptic cleft, leading to increased synaptic concentrations and prolonged effects. It is a potent local anesthetic and has a high abuse potential.
Mechanism of Action:
Blockade of Neurotransmitter Reuptake: Cocaine primarily blocks the reuptake of neurotransmitters such as dopamine, norepinephrine, and serotonin from the synaptic clefts in the brain. This leads to an increase in the concentration of these neurotransmitters in the brain, resulting in heightened mood, increased energy, and euphoria.
Local Anesthetic: Cocaine also acts as a local anesthetic by blocking sodium channels, thereby inhibiting the propagation of nerve impulses and producing numbness in the area of application.
– Atomoxetine: Selectively inhibits the reuptake of norepinephrine, primarily used in the treatment of ADHD.
Mechanism of Action: Atomoxetine works by inhibiting the reuptake of norepinephrine, which increases its concentration in the synaptic clefts of neurons in the brain. This modulation of norepinephrine levels helps improve attention, reduce impulsiveness, and control hyperactivity in individuals with ADHD.
3. Mixed-Acting Agonists
Mixed-acting sympathomimetics stimulate both alpha and beta-adrenergic receptors to varying degrees, producing a broader range of effects.
– Epinephrine (Adrenaline): Acts on both alpha- and beta-adrenergic receptors. It increases heart rate, cardiac output, and blood pressure, while also dilating bronchioles and improving airway patency. Used in anaphylaxis, cardiac arrest, and severe asthma attacks.
Mechanism of Action:
Adrenergic Receptor Agonist: Epinephrine acts on both alpha and beta adrenergic receptors in the sympathetic nervous system.
Alpha-adrenergic receptors: Stimulation leads to vasoconstriction, which increases blood pressure and redirects blood flow to vital organs.
Beta-adrenergic receptors:
Beta-1 receptors: Stimulation increases heart rate (positive chronotropic effect), contractility (positive inotropic effect), and conduction velocity (positive dromotropic effect).
Beta-2 receptors: Stimulation causes relaxation of smooth muscles in the bronchioles (bronchodilation) and blood vessels (vasodilation in skeletal muscle and liver).
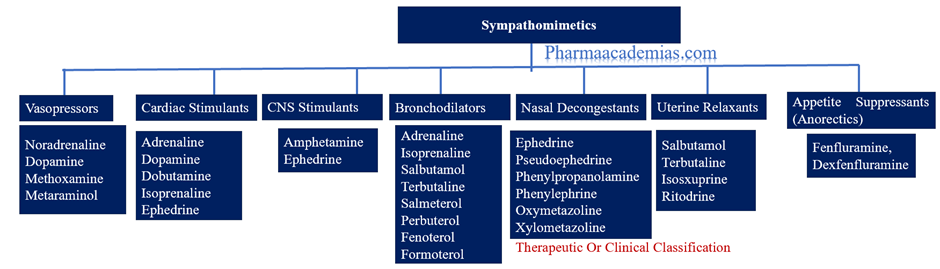
Clinical Uses
Sympathomimetic drugs are used clinically for various purposes:
– Cardiovascular: Treatment of hypotension (phenylephrine), bradycardia (isoproterenol), and cardiac arrest (epinephrine).
– Respiratory: Bronchodilation in asthma and COPD (salbutamol).
– Central Nervous System: Treatment of ADHD and narcolepsy (amphetamine).
– Local Anesthesia: Cocaine as a local anesthetic.
– Emergency Medicine: Epinephrine for anaphylaxis and acute severe asthma.
Understanding the classification and mechanisms of action of sympathomimetics is crucial for their safe and effective use in clinical practice, considering their diverse effects on different adrenergic receptors throughout the body.

