Cell damage can be either reversible or irreversible, depending on the extent and severity of the injury. When the cellular response is adaptive, homeostasis is maintained, and the damage can be repaired. However, when the injury (or stress) is too severe for the cell to repair itself, cell death ensues. The outcome of cell injury depends on the duration of exposure to the harmful stimulus and the severity of the damage caused. Cell death can manifest through several mechanisms, such as severe cell swelling or rupture, denaturation and coagulation of cytoplasmic proteins, and breakdown of cell organelles (necrosis), or through internally controlled processes like chromatin condensation and fragmentation (apoptosis).
Reversible and Irreversible Cell Injury:
Reversible Cell Injury: This occurs when the injury is mild or short-term. If the damaging stimulus is removed, cells can recover and return to their normal state, maintaining structural and functional integrity.
Irreversible Cell Injury (Cell Death): This occurs when the injury is too severe or prolonged, leading to cell death. Irreversible cell injury can result from:
Necrosis: Characterized by cell swelling, rupture, denaturation and coagulation of proteins, and breakdown of organelles, leading to inflammation.
Apoptosis: Involves chromatin condensation and fragmentation, a controlled, energy-dependent process that does not elicit inflammation.
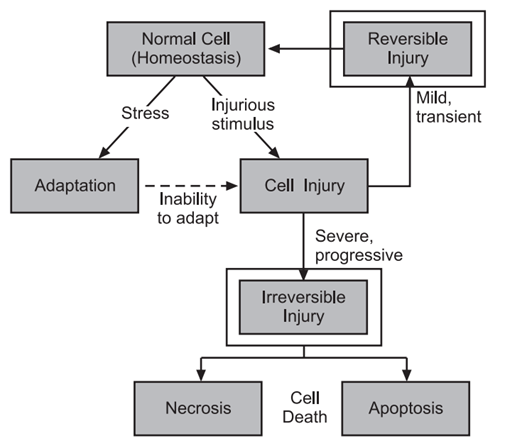
Cellular Responses to Injury
The response of cells to injurious stimuli depends on the type, duration, and severity of the injury. For example:
Low doses of toxins or brief ischemia: May lead to reversible cell injury.
High doses of toxins or prolonged ischemia: May cause irreversible injury and cell death.
Factors Influencing Cell Injury
The outcome of cell injury is influenced by several factors, including:
Type of Cell: Different cell types have different sensitivities to injury. For instance, skeletal muscle cells can endure complete ischemia for 2-3 hours, while cardiac muscle cells can only withstand it for 20-30 minutes.
Status and Adaptability: The nutritional and hormonal status of cells affects their response to injury. For example, glycogen-replete hepatocytes can better tolerate ischemia than those that are depleted of glucose.
Genetic Makeup: Genetic diversity in metabolic pathways can influence the response to toxins. Individuals with different variants in genes encoding enzymes like cytochrome P-450 may metabolize toxins at different rates, leading to varied outcomes. Understanding genetic polymorphisms is crucial for predicting responses to drugs and toxins and for assessing disease susceptibility.
Targets of Injurious Stimuli:
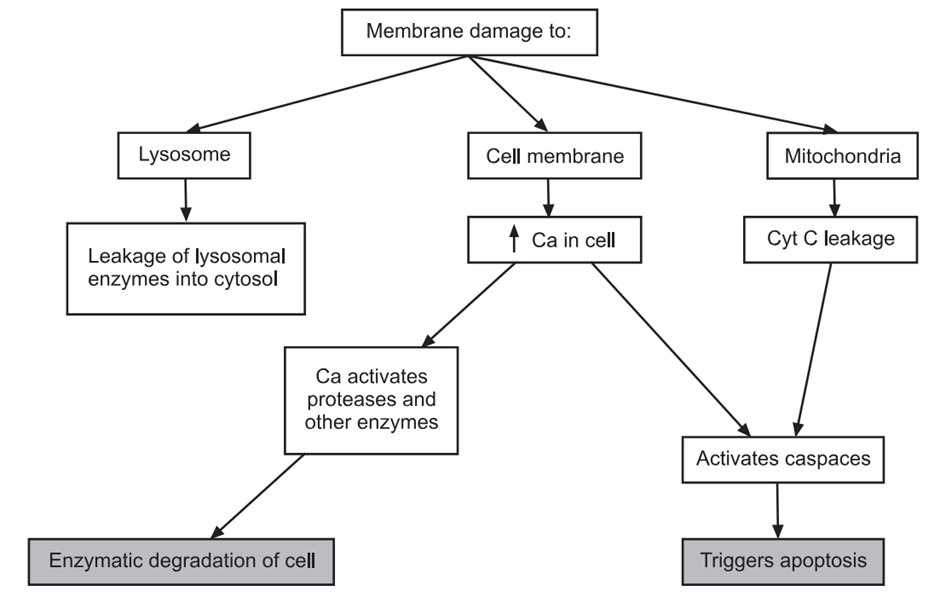
Cell injury results from functional and biochemical abnormalities in essential cellular components. The most critical targets include:
Mitochondria: Sites of ATP generation. Damage to mitochondria can lead to energy depletion and cell death.
Cell Membranes: Maintain ionic and osmotic homeostasis. Damage to membranes disrupts cellular integrity and function.
Protein Synthesis: Essential for cell maintenance and repair. Disruption can impair cell function and survival.
Cytoskeleton: Provides structural support and facilitates intracellular transport. Damage can lead to cell dysfunction.
Genetic Apparatus: Includes DNA and associated machinery. Damage can result in mutations and cell death.
In summary, the pathogenesis of cell injury involves a complex interplay of factors that determine whether a cell can adapt to or succumb to stress. Understanding these mechanisms is crucial for developing effective therapeutic strategies to prevent and treat cellular and tissue damage.

