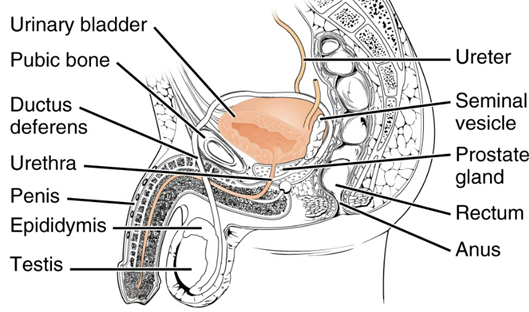
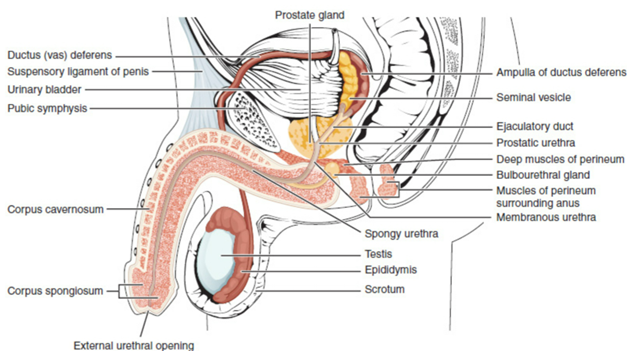
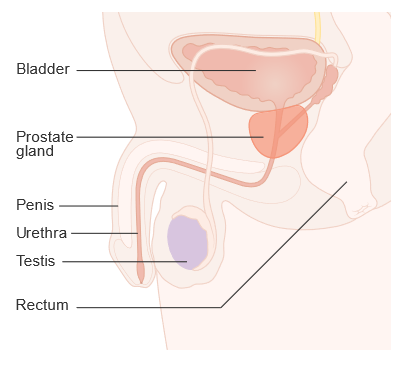
The male reproductive system is a complex network of organs, glands, and ducts that work together to produce, maintain, and transport sperm, the male reproductive cells, and to produce male sex hormones. Understanding its anatomy and functions is crucial for comprehending male reproductive health and physiology.
Anatomy of the Male Reproductive System
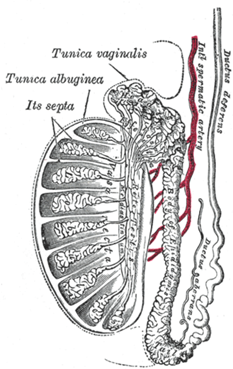
1. Testes (Testicles):
The testes, or testicles, are the primary male reproductive organs located within the scrotum, a skin-covered sac that hangs outside the abdominal cavity. Each testis is an oval-shaped organ approximately 4-5 cm long, 3 cm wide, and 2.5 cm thick. The testes are divided into lobules, which contain tightly coiled seminiferous tubules where spermatogenesis, the production of sperm, occurs. Within these tubules, spermatogenic cells undergo a series of transformations, including mitosis and meiosis, to become mature sperm cells.
Additionally, the testes house Leydig cells, which are located in the interstitial spaces between the seminiferous tubules. These cells are responsible for producing testosterone, the principal male sex hormone essential for the development of male secondary sexual characteristics and the regulation of spermatogenesis.

– Function: The primary functions of the testes are the production of sperm (spermatogenesis) and the synthesis of testosterone, the principal male sex hormone.
2. Scrotum:
The scrotum is a sac of skin and muscle situated behind the penis, which plays a crucial role in regulating the temperature of the testes. It is divided into two compartments, each containing one testis. The scrotum maintains the testes at a temperature approximately 2-3°C below the core body temperature, which is necessary for the proper development of sperm. This temperature regulation is achieved through the action of the cremaster muscle, which contracts to raise the testes closer to the body in cold conditions and relaxes to lower them away from the body in warmer conditions.
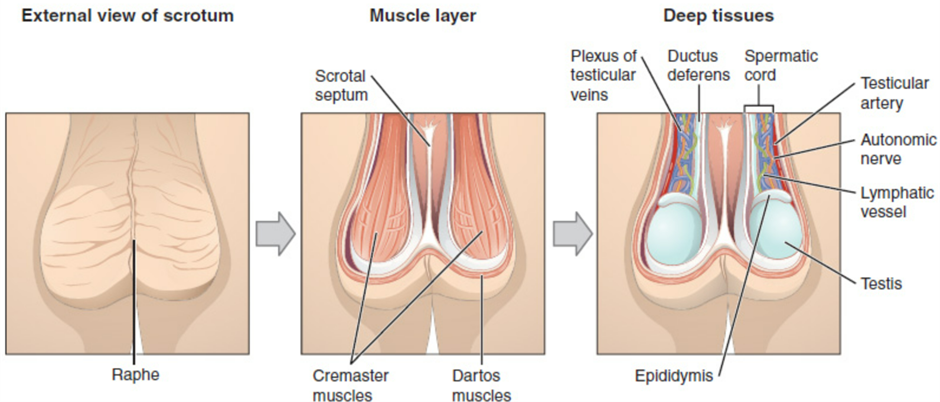
– Function: Regulates the temperature of the testes, keeping them slightly cooler than body temperature, which is necessary for optimal sperm production.
3. Epididymis:
The epididymis is a long, coiled tube that is attached to the back of each testis. It is composed of three sections: the head, body, and tail. The head receives immature sperm from the efferent ducts of the testes. As sperm travel through the body and tail of the epididymis, they undergo further maturation, gaining motility and the ability to fertilize an egg. The epididymis also serves as a storage site for mature sperm until they are transported during ejaculation.
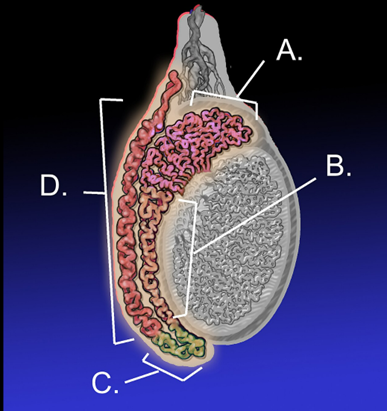
– Function: Stores and matures sperm cells produced in the testes. It also absorbs fluid and recycles damaged sperm cells.
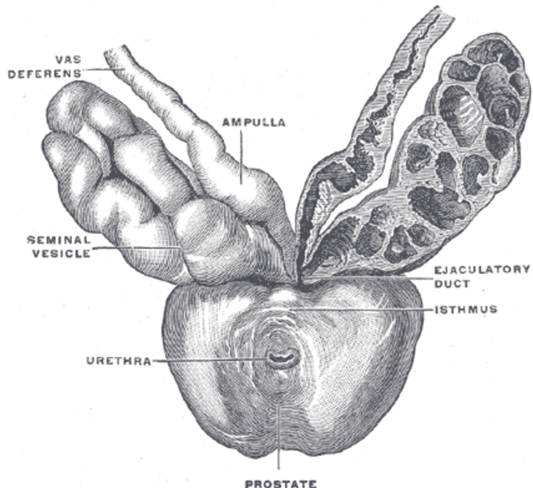
4. Vas Deferens (Ductus Deferens):
The vas deferens, or ductus deferens, is a muscular tube approximately 45 cm long that extends from the tail of the epididymis to the ejaculatory ducts. Its primary function is to transport mature sperm from the epididymis to the ejaculatory ducts in preparation for ejaculation. This transportation is facilitated by peristaltic contractions of the smooth muscle in the walls of the vas deferens.
the arrangement of the ducts
– Function: Transports mature sperm to the urethra in preparation for ejaculation.
5. Ejaculatory Ducts:
The ejaculatory ducts are formed by the fusion of the vas deferens and the seminal vesicles. They pass through the prostate gland and open into the urethra. During ejaculation, the ejaculatory ducts mix sperm from the vas deferens with seminal fluid from the seminal vesicles, forming semen. This mixture then travels through the urethra for expulsion from the body.
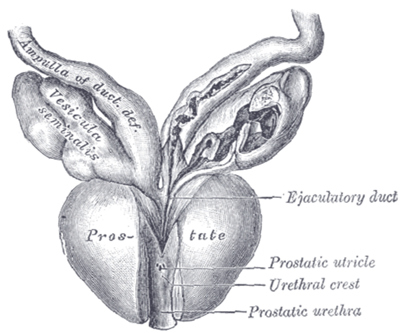
– Function: Mix sperm with fluids from the seminal vesicles and transport them to the urethra.
6. Urethra:
The urethra is a tube that runs from the bladder through the penis, serving dual functions in the male reproductive and urinary systems. It is divided into three parts: the prostatic urethra, which passes through the prostate gland; the membranous urethra, which passes through the urogenital diaphragm; and the penile (spongy) urethra, which runs along the length of the penis. The urethra transports both urine from the bladder and semen from the reproductive ducts, though not simultaneously.
– Function: Conveys both urine and semen to the exterior of the body but not simultaneously.
7. Penis:
The penis is the external male sexual organ composed of the root, body (shaft), and glans penis. It contains three columns of erectile tissue: two corpora cavernosa on the dorsal side and one corpus spongiosum on the ventral side, which surrounds the urethra. During sexual arousal, the erectile tissues fill with blood, causing the penis to become rigid and erect. This rigidity allows the penis to deliver semen into the female reproductive tract during intercourse.
– Function: Delivers semen into the female reproductive tract during sexual intercourse. The erectile tissue allows the penis to become rigid and erect.
8. Seminal Vesicles:
The seminal vesicles are paired glands located behind the bladder and above the prostate gland. They produce seminal fluid, which is rich in fructose, prostaglandins, and proteins. This fluid constitutes about 60-70% of the total volume of semen and provides energy for the sperm, enhances their motility, and helps neutralize the acidic environment of the female reproductive tract.
– Function: Produce seminal fluid, which is rich in fructose, prostaglandins, and proteins. This fluid constitutes about 60-70% of the total volume of semen and provides energy for the sperm.
9. Prostate Gland:
The prostate gland is a walnut-sized gland located below the bladder and surrounding the urethra. It secretes prostate fluid, one of the components of semen, which contains enzymes, citric acid, and prostate-specific antigen (PSA). This fluid helps to thin the semen, improving sperm motility and longevity, and also neutralizes the acidic environment of the urethra and the female reproductive tract.
– Function: Secretes prostate fluid, one of the components of semen. This fluid contains enzymes, citric acid, and prostate-specific antigen (PSA), which help in sperm motility and longevity.
10. Bulbourethral Glands (Cowper’s Glands):
The bulbourethral glands, also known as Cowper’s glands, are small, pea-sized glands located below the prostate and at the base of the penis. These glands secrete a clear, mucus-like fluid during sexual arousal, which precedes the ejaculation of semen. This pre-ejaculate fluid lubricates the urethra, neutralizes any residual acidity from urine, and provides a more favorable environment for the passage of sperm.
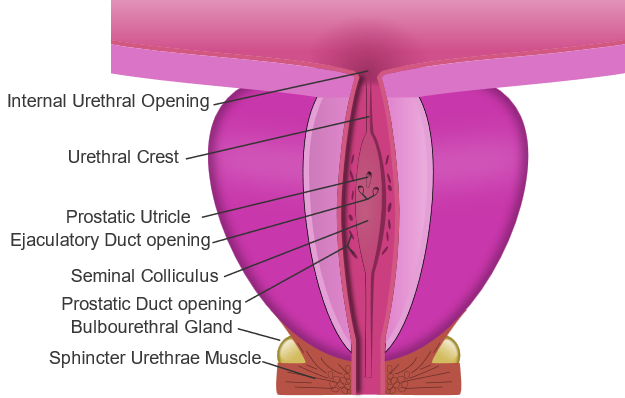
– Function: Secrete a clear, mucus-like fluid during sexual arousal. This pre-ejaculate fluid lubricates the urethra and neutralizes any acidity from residual urine, creating a more favorable environment for sperm.
Functions of the Male Reproductive System
1. Spermatogenesis:
– Process: Takes place within the seminiferous tubules of the testes. It involves the production of haploid sperm cells from diploid spermatogonia through mitosis and meiosis.
– Hormonal Regulation: Controlled by the hypothalamic-pituitary-gonadal axis. GnRH from the hypothalamus stimulates the release of FSH and LH from the pituitary gland. FSH stimulates spermatogenesis, while LH stimulates testosterone production.
2. Testosterone Production:
– Source: Produced by Leydig cells located between the seminiferous tubules in the testes.
– Functions: Essential for the development of male secondary sexual characteristics (e.g., facial hair, deep voice), maintenance of libido, promotion of spermatogenesis, and overall male reproductive health.
3. Sperm Maturation and Storage:
– Epididymis: Sperm mature as they travel through the epididymis, gaining motility and the ability to fertilize an egg. Mature sperm are stored in the tail of the epididymis until ejaculation.
4. Semen Production:
– Seminal Vesicles and Prostate Gland: Contribute fluids that nourish and protect sperm, facilitating their motility and viability.
– Bulbourethral Glands: Provide lubricating fluid to facilitate sperm passage and neutralize the acidic environment of the urethra.
5. Erection and Ejaculation:
– Erection: Achieved by the engorgement of erectile tissues in the penis with blood. This process is mediated by parasympathetic nervous system stimulation, which causes the release of nitric oxide, leading to vasodilation.
– Ejaculation: Involves two phases: emission (movement of semen into the urethra) and expulsion (forcible ejection of semen from the urethra). Controlled by the sympathetic nervous system.
Understanding the male reproductive system’s anatomy and functions provides insight into its role in human reproduction and the importance of maintaining reproductive health. Any disruption in these processes can lead to fertility issues and other health problems, making this knowledge crucial for both medical professionals and individuals.

