Spermatogenesis is the process by which male germ cells, called spermatogonia, undergo transformation into mature spermatozoa (sperm cells). It is a complex and tightly regulated process that occurs within the seminiferous tubules of the testes. Understanding spermatogenesis is crucial for comprehending male fertility, reproductive health, and the development of treatments for male infertility.
Overview of Spermatogenesis
Spermatogenesis can be broadly divided into three main phases: mitotic division, meiotic division, and spermiogenesis.
1. Mitotic Division (Proliferation Phase)
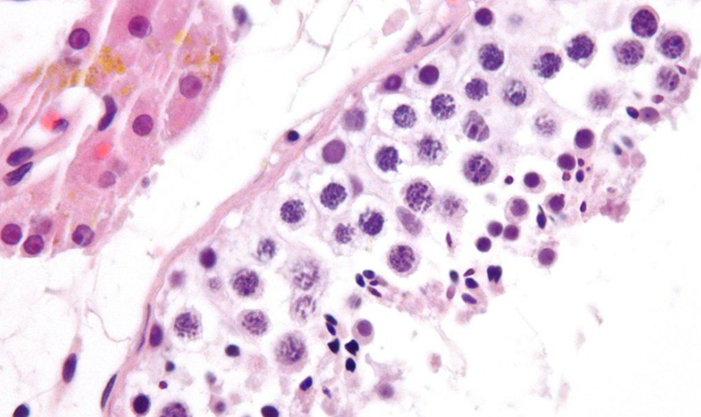
– Spermatogonia: Spermatogenesis begins with spermatogonia, which are undifferentiated diploid stem cells located in the outermost layer of the seminiferous tubules.
– Type A Spermatogonia: These are the stem cells that maintain the germ cell line and undergo self-renewal through mitotic divisions.
– Type B Spermatogonia: These cells are derived from type A spermatogonia and differentiate into primary spermatocytes.
2. Meiotic Division (Maturation Phase)
– Primary Spermatocytes: Type B spermatogonia differentiate into primary spermatocytes, which are diploid (2n) cells.
– Meiosis I: Each primary spermatocyte undergoes meiosis I, resulting in the formation of two secondary spermatocytes, which are haploid (n) cells.
– Meiosis II: Each secondary spermatocyte then undergoes meiosis II to produce four haploid spermatids.
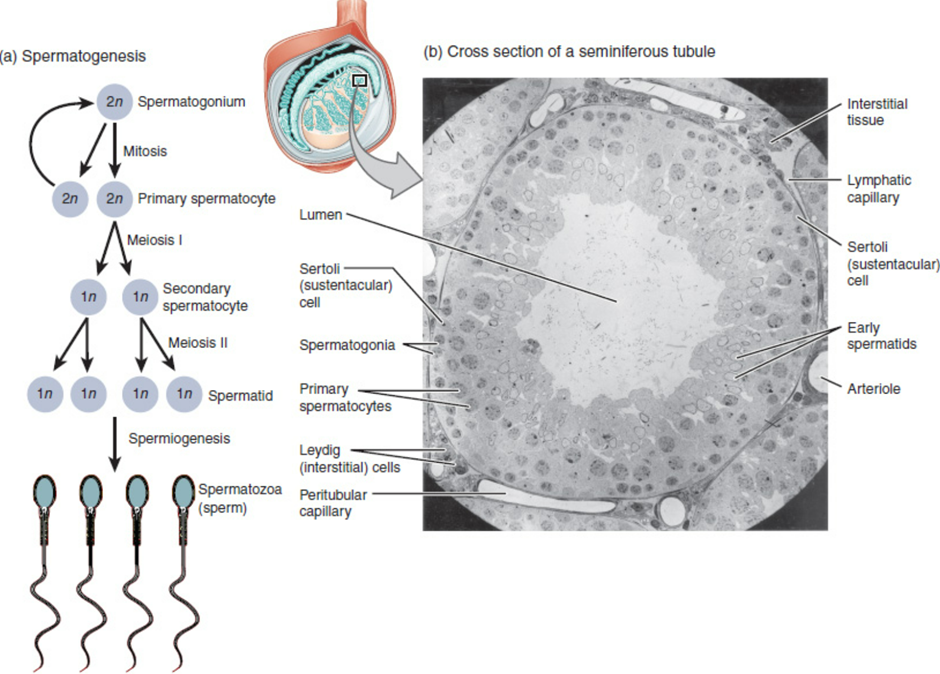
3. Spermiogenesis (Differentiation Phase)
– Spermatids: Spermiogenesis is the final phase of spermatogenesis, during which haploid spermatids undergo a series of structural and functional changes to differentiate into mature spermatozoa.
– Golgi Phase: The Golgi apparatus forms the acrosome, a cap-like structure containing enzymes essential for fertilization.
– Cap Phase: The centrioles migrate to the opposite pole of the nucleus, forming the neck and tail of the sperm.
– Acrosomal Phase: The nucleus elongates and condenses, and the mitochondria aggregate around the flagellum to provide energy for motility.
– Maturation Phase: The excess cytoplasm is shed, and the spermatozoa are released into the lumen of the seminiferous tubules.
Hormonal Regulation of Spermatogenesis
Spermatogenesis is tightly regulated by the hypothalamic-pituitary-gonadal (HPG) axis, involving several key hormones:
– Gonadotropin-Releasing Hormone (GnRH): Secreted by the hypothalamus, GnRH stimulates the anterior pituitary gland to release gonadotropins.
– Follicle-Stimulating Hormone (FSH): Stimulates Sertoli cells within the seminiferous tubules to support spermatogenesis, including the regulation of spermatogonial proliferation and the production of androgen-binding protein (ABP).
– Luteinizing Hormone (LH): Stimulates Leydig cells in the interstitial tissue of the testes to produce testosterone.
– Testosterone: Produced by Leydig cells, testosterone is essential for spermatogenesis, promoting the development and maintenance of male secondary sexual characteristics and supporting spermatogenic function.
Cellular Architecture of the Testis
The testes are composed of seminiferous tubules and interstitial tissue:
– Seminiferous Tubules: These are highly coiled tubules where spermatogenesis occurs. They are lined with Sertoli cells that provide structural support and nourishment to developing germ cells.
– Interstitial Tissue: Found between seminiferous tubules, this tissue contains Leydig cells, blood vessels, and connective tissue. Leydig cells produce testosterone in response to LH stimulation.
Factors Influencing Spermatogenesis
Several factors can influence the process of spermatogenesis:
– Temperature: Spermatogenesis is temperature-sensitive, requiring a slightly lower temperature than body temperature. The scrotum and cremaster muscle help regulate testicular temperature.
– Hormonal Imbalances: Disorders affecting the HPG axis, such as hypogonadism or hyperprolactinemia, can disrupt spermatogenesis.
– Genetic Factors: Genetic mutations or chromosomal abnormalities, such as Klinefelter syndrome (XXY), can impair spermatogenesis.
– Environmental Factors: Exposure to toxins, radiation, heat, or certain medications can adversely affect spermatogenesis.
Clinical Relevance and Disorders
Understanding spermatogenesis is essential for diagnosing and treating male infertility and reproductive disorders:
– Male Infertility: Disorders affecting spermatogenesis, such as oligospermia (low sperm count), asthenospermia (poor sperm motility), or teratospermia (abnormal sperm morphology), can contribute to male infertility.
– Treatment Approaches: Therapeutic strategies for male infertility may include hormonal therapies, lifestyle modifications, surgical interventions, or assisted reproductive technologies (ART) such as intracytoplasmic sperm injection (ICSI) or in vitro fertilization (IVF).
– Research and Development: Continued research into spermatogenesis mechanisms and regulatory pathways informs advancements in male reproductive health, fertility preservation, and contraceptive development.
Conclusion
Spermatogenesis is a complex and highly regulated process that ensures the continuous production of functional spermatozoa for male fertility. It involves sequential phases of mitotic and meiotic divisions, followed by spermiogenesis to transform spermatids into mature spermatozoa. Hormonal regulation by the HPG axis, cellular interactions within the testes, and environmental factors all contribute to the process of spermatogenesis. Understanding the intricacies of spermatogenesis is crucial for diagnosing and managing male reproductive health conditions and advancing treatments for male infertility. Continued research into spermatogenesis promises further insights into male fertility and reproductive medicine.