Absorption of Drugs from Non-Per-Oral
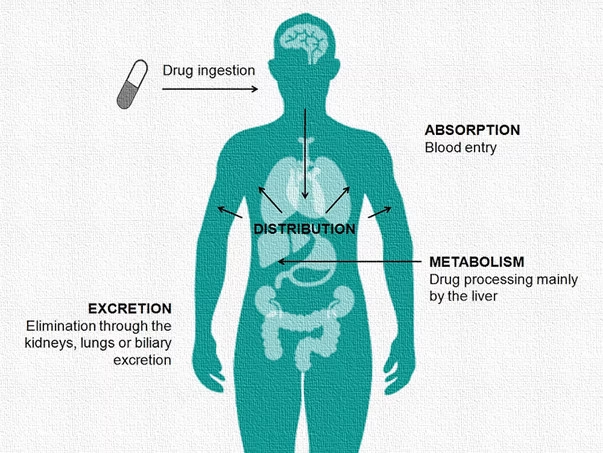
Absorption of Drugs from Non-Per-Oral: Drug administration via non-per-oral extravascular routes refers to delivering therapeutic agents into the body through alternative pathways that do not involve the gastrointestinal tract or direct vascular access (such as intravenous or intra-arterial routes). These methods are employed to bypass challenges like poor oral bioavailability, gastrointestinal degradation, extensive first-pass hepatic metabolism, or when immediate therapeutic action is required. Each of these routes presents a unique anatomical, physiological, and biochemical environment, affecting how a drug is absorbed into systemic circulation.
1. Intramuscular (IM) Absorption
Intramuscular administration involves injecting the drug deep into large skeletal muscle masses such as the deltoid, vastus lateralis, or gluteus maximus. Once the drug is deposited in the muscle tissue, it must traverse the extracellular matrix and capillary walls to reach systemic circulation.
- Perfusion-dependent process: The rate and extent of absorption are significantly influenced by the vascularity of the muscle. Highly perfused areas lead to faster absorption.
- Formulation types: Aqueous solutions typically get absorbed within 10–30 minutes, while depot or oil-based suspensions release the drug slowly over hours, days, or even weeks.
- Influence of muscle activity: Exercise or massage at the injection site can increase local blood flow, thus accelerating the absorption process.
- Drug properties: Water-soluble and small molecular weight drugs exhibit faster uptake.
- Depot advantage: Some drugs (e.g., antipsychotics like fluphenazine decanoate) are designed for slow and sustained release from intramuscular depots to ensure prolonged therapeutic levels.

2. Subcutaneous (SC) Absorption
Subcutaneous administration involves injecting the drug into the adipose tissue layer beneath the dermis but above the muscle layer. This route is commonly used for drugs requiring slow and continuous absorption.
- Lower perfusion compared to muscle: This causes a slower rate of absorption compared to IM injections, though variability exists based on the site (abdomen, thigh, arm).
- Absorption kinetics: Drugs absorbed via SC routes typically exhibit a more gradual onset but can achieve relatively consistent plasma levels over time.
- Formulation and enzyme action: Peptides and proteins like insulin are susceptible to enzymatic degradation by proteases, and their absorption can be incomplete or variable.
- Specialized devices: Pen injectors and insulin pumps help maintain therapeutic levels with convenience and minimal invasiveness.
- Depot systems: Long-acting formulations like leuprolide acetate use bioerodible polymers to prolong drug release.

3. Transdermal (TD) Absorption
Transdermal drug delivery is achieved by applying a formulation directly onto the skin surface, from where the drug penetrates through various skin layers into systemic circulation.
- Barrier function of the stratum corneum: This outermost layer acts as the principal obstacle to absorption. Only lipophilic, small molecular weight drugs (<500 Da) can passively diffuse through.
- Enhanced permeability: Use of chemical enhancers (e.g., ethanol, DMSO), physical enhancers (microneedles, iontophoresis), or formulation innovations (liposomes, nanoemulsions) helps facilitate permeation.
- Controlled-release systems: Transdermal patches like those for fentanyl or clonidine deliver the drug steadily over several hours to days, ensuring a consistent plasma concentration.
- Site of application: Areas with thinner skin and higher perfusion, such as behind the ears or the upper chest, improve drug absorption.
- Bypassing hepatic metabolism: Transdermal administration avoids first-pass hepatic metabolism, improving bioavailability of susceptible drugs.

4. Inhalational (Pulmonary) Absorption
Inhalation route utilizes the vast surface area of the lungs and their rich vascular supply to rapidly deliver drugs into the systemic circulation or directly to lung tissues for local effect.
- Alveolar surface advantages: The lungs offer an enormous absorptive area (approximately 70–100 m²) and a thin alveolar-capillary barrier, which allows for the rapid transfer of lipophilic drugs into the bloodstream.
- Particle size criticality: Particles sized 1–5 microns reach the deep lung (alveoli), whereas larger particles may get trapped in the oropharynx or upper airways, reducing bioavailability.
- Aerosol systems: Metered-dose inhalers, dry powder inhalers, and nebulizers are used for drug delivery depending on the therapeutic need and formulation.
- Rapid systemic effect: This is especially important for anesthetic gases like isoflurane, sevoflurane, or emergency bronchodilators like salbutamol.
- Avoidance of first-pass metabolism: Drugs administered via the pulmonary route escape hepatic first-pass degradation, improving therapeutic outcomes, especially for peptides or hormones.

5. Rectal Absorption
Rectal administration is achieved by placing the drug (in the form of suppositories, enemas, or gels) into the rectum, where it can be absorbed through the rectal mucosa.
- Partial avoidance of first-pass effect: The lower and middle rectal veins drain directly into the systemic circulation (inferior and middle rectal veins), bypassing the liver, whereas the upper rectal vein drains into the portal circulation.
- Physiological conditions affecting absorption: Absorption is influenced by rectal fluid content, pH (typically neutral to slightly alkaline), and the presence of fecal matter.
- Formulation characteristics: Lipophilic suppository bases like cocoa butter melt at body temperature, while hydrophilic bases like PEG dissolve to release the drug.
- Clinical utility: Especially useful in pediatric or unconscious patients, or when oral administration is contraindicated due to vomiting or dysphagia.
- Examples of rectally administered drugs: Diazepam (for seizures), paracetamol (for fever), and bisacodyl (as a laxative).

6. Vaginal Absorption
Vaginal drug delivery involves administration through vaginal suppositories, pessaries, gels, tablets, or rings for both local and systemic therapeutic effects.
- Highly vascular mucosa: The vaginal mucosa permits absorption of both hydrophilic and lipophilic drugs, especially when formulations enhance contact time.
- Effect of hormonal variations: Estrogen levels influence epithelial thickness and vascularity, affecting permeability and drug absorption.
- Formulation diversity: Bioadhesive systems, thermosensitive gels, and controlled-release vaginal rings (e.g., NuvaRing for contraception) enhance drug residence and delivery.
- First-pass metabolism avoidance: Vaginal administration circumvents the hepatic first-pass effect, leading to better systemic bioavailability of certain drugs.
- Therapeutic applications: Used for local infections (e.g., miconazole for candidiasis), hormone replacement therapy (e.g., estradiol), and systemic effects like contraception.

7. Nasal Absorption
Intranasaladministration utilizes the highly vascular nasal mucosa to deliver drugs for local or systemic effects.
- Anatomical advantages: The nasal cavity provides a large surface area (~150 cm²) and rapid blood flow, making it ideal for systemic delivery of rapidly acting drugs.
- Rapid onset and non-invasiveness: This route is particularly suitable for emergencies (e.g., naloxone for opioid overdose) or for drugs that are degraded in the gastrointestinal tract.
- Formulation considerations: Spray viscosity, particle size, pH (ideally between 4.5 and 6.5), and osmolarity influence absorption.
- Challenges: Ciliary clearance and mucosal enzymatic degradation can reduce drug bioavailability. Strategies like mucoadhesive polymers and enzyme inhibitors help improve drug uptake.
- Emerging uses: Intranasal delivery of vaccines, peptides (like calcitonin), and CNS-acting drugs (targeting the brain via the olfactory nerve pathway).

8. Ocular (Ophthalmic) Absorption
Ophthalmic drug delivery is mainly intended for local treatment within the eye but can lead to systemic absorption via the conjunctival sac and nasolacrimal drainage.
- Absorption pathways: Drugs can enter systemic circulation through conjunctival blood vessels or nasal mucosa after draining via the nasolacrimal duct.
- Barriers to absorption: The eye’s natural defenses, including blinking, tear production, and corneal epithelium, limit drug retention and absorption.
- Formulation innovations: To overcome rapid clearance, sustained-release inserts, in situ gels, nanoparticles, and microemulsions are used.
- Systemic side effects: Though the target is usually local (e.g., for glaucoma, conjunctivitis), unintended systemic effects (like bradycardia from timolol) may occur.
- Clinical applications: Delivery of antibiotics (e.g., ciprofloxacin), antiglaucoma agents (e.g., latanoprost), and anti-inflammatory medications.

9. Buccal and Sublingual Absorption
Buccal and sublingual routes involve placing drugs in the oral cavity, either in the cheek pouch (buccal) or beneath the tongue (sublingual), for rapid systemic absorption through the rich venous drainage of the oral mucosa.
- High vascularity and thin epithelium: These allow rapid drug diffusion into the bloodstream, bypassing hepatic first-pass metabolism.
- Drug characteristics: Ideal candidates are lipophilic, potent, and small molecules, as the oral mucosa has limited permeability compared to the intestine.
- Formulation types: Sublingual tablets (e.g., nitroglycerin), buccal patches (e.g., buprenorphine), mucoadhesive films, and lozenges.
- Saliva-dependent dissolution: Drug absorption depends on dissolution in the minimal saliva volume, making pH and enzymatic stability critical factors.
- Therapeutic uses: Effective for angina (e.g., nitroglycerin), hormone therapy (e.g., testosterone buccal tablets), and analgesia.
Conclusion
Each non-per-oral extravascular route of drug administration offers unique advantages tailored to specific clinical needs, patient populations, and pharmacokinetic goals. The choice of route is influenced by the drug’s physicochemical properties, desired speed of onset, duration of action, systemic bioavailability, and the feasibility of administration. Understanding the anatomical, physiological, and formulation-related aspects of these routes allows for better design and optimization of therapeutic regimens, ensuring maximum efficacy with minimal side effects.

