Antiarrhythmic drugs are medications designed to prevent, control, or manage abnormal heart rhythms, known as arrhythmias. Arrhythmias are disturbances in the normal electrical activity of the heart, which can cause the heart to beat too quickly (tachycardia), too slowly (bradycardia), or irregularly.
Classification of Antiarrhythmic drugs
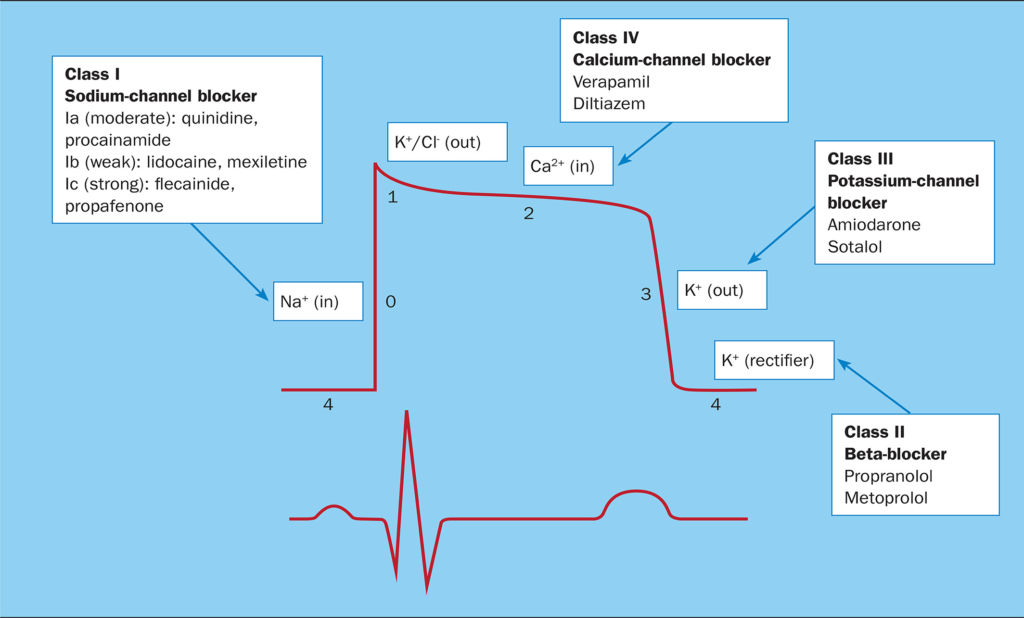
Anti-arrhythmic drugs are classified into four main classes based on their mechanism of action according to the Vaughan-Williams classification:
Class I. Sodium Channel Blockers
These drugs primarily affect the sodium channels during the cardiac action potential. They are further subdivided into three subclasses based on their effects on repolarization:
A. Prolong Repolarization:
1. Quinidine: Used for atrial and ventricular arrhythmias.
2. Procainamide: Particularly effective for ventricular arrhythmias.
3. Disopyramide: Primarily used for atrial arrhythmias.
B. Shorten Repolarization:
1. Lignocaine (Lidocaine): Mainly used for ventricular arrhythmias associated with acute myocardial infarction.
2. Mexiletine: Similar to lignocaine, used for ventricular arrhythmias.
3. Phenytoin: Can be used for ventricular arrhythmias, especially in digitalis toxicity.
C. Little Effect on Repolarization:
1. Encainide: Previously used for ventricular arrhythmias but discontinued in many countries due to safety concerns.
2. Flecainide: Primarily used for supraventricular arrhythmias and certain ventricular arrhythmias.
3. Propafenone: Used for atrial fibrillation/flutter and certain ventricular arrhythmias.
Class II. β-adrenergic Blockers (Reduce Sympathetic Tone)
These drugs primarily block beta-adrenergic receptors, reducing the effects of sympathetic stimulation on the heart. Common examples include:
Propranolol: Used for a wide range of arrhythmias, angina, and hypertension.
Acebutolol: Combines beta-blocking and mild antiarrhythmic properties.
Esmolol: Has a short duration of action and is often used in acute settings.
Class III. K+ Channel Blockers (Prolong Repolarization)
These drugs prolong the repolarization phase of the cardiac action potential, primarily by blocking potassium channels. Notable examples include:
Amiodarone: Used for various arrhythmias but has a broad range of potential side effects.
Bretylium: Used in certain life-threatening ventricular arrhythmias.
Sotalol: Combines beta-blocking and potassium channel-blocking properties.
Dofetilide: Used for atrial fibrillation/flutter.
Ibutilide: Used for acute termination of atrial fibrillation/flutter.
Class IV. Ca++ Channel Blockers (Prolong Conduction and Refractoriness, Especially in SA and AV Nodes)
These drugs inhibit calcium influx during the action potential, affecting the contractility of the heart and slowing down the heart rate. Examples include:
Verapamil: Used for supraventricular arrhythmias and hypertension.
Diltiazem: Similar to verapamil, used for supraventricular arrhythmias and certain forms of angina.
These antiarrhythmic drugs are crucial components of arrhythmia management, and their use requires careful consideration of the specific arrhythmia type, patient characteristics, and potential side effects. Regular monitoring is often necessary to ensure optimal therapeutic outcomes.
Pharmacological Actions of Anti-Arrhythmic Drugs
Class I (Sodium Channel Blockers): These drugs affect the sodium channels in cardiac cells, altering the depolarization phase of the action potential.
Class II (Beta-Adrenergic Blockers): By blocking beta receptors, they decrease the effects of sympathetic stimulation, reducing heart rate and contractility.
Class III (Potassium Channel Blockers): These drugs prolong the action potential duration by delaying repolarization.
Class IV (Calcium Channel Blockers): They inhibit calcium influx during the action potential, affecting the contractility of the heart and slowing down the heart rate.
Dose of Anti-Arrhythmic Drugs
Dosing varies widely among anti-arrhythmic drugs and depends on the specific medication, the patient’s condition, and individual response. Dosages are typically initiated at lower levels and adjusted based on the patient’s response and tolerance.
Indications of Anti-Arrhythmic Drugs
Atrial Fibrillation (AF) and Atrial Flutter: These are fast and irregular heart rhythms starting in the upper chambers (atria) of the heart. Anti-arrhythmic drugs are used to either slow the heart rate (rate control) or to restore and maintain a normal rhythm (rhythm control).
Supraventricular Tachycardia (SVT): A rapid heart rate originating above the ventricles (lower chambers). Drugs like adenosine, beta-blockers, and calcium channel blockers are used for quick termination or prevention.
Ventricular Tachycardia (VT) and Ventricular Fibrillation (VF): Life-threatening rhythms starting from the ventricles. Medications like amiodarone or lidocaine are used during emergencies or to prevent recurrence.
Wolff-Parkinson-White (WPW) Syndrome: A condition with an extra electrical pathway in the heart, causing fast heartbeats. Certain anti-arrhythmic drugs help prevent episodes.
Post-Myocardial Infarction (Post-MI) Arrhythmias: After a heart attack, patients are at increased risk of arrhythmias. Some anti-arrhythmic drugs help reduce this risk.
Long QT Syndrome: A disorder of the heart’s electrical activity that can cause sudden, dangerous arrhythmias. Beta-blockers are commonly used.
Heart Failure with Arrhythmia: In patients with heart failure, some drugs like digoxin or amiodarone can help manage the heart rhythm.
Contraindications of Anti-Arrhythmic Drugs
Structural Heart Disease: Class IC drugs (like Flecainide, Propafenone) are contraindicated in patients with structural heart disease (e.g., previous heart attack, cardiomyopathy) due to risk of life-threatening arrhythmias.
Heart Block or Bradycardia (Slow Heart Rate): Drugs that slow conduction (e.g., beta-blockers, calcium channel blockers, digoxin) should be avoided in patients with AV block or bradycardia unless a pacemaker is present.
Severe Heart Failure: Class I and some Class III drugs (except amiodarone) can worsen heart failure and are contraindicated. Verapamil and diltiazem (Class IV) are also contraindicated in heart failure.
Asthma or COPD (Chronic Obstructive Pulmonary Disease): Non-selective beta-blockers (like propranolol) can worsen bronchospasm and are contraindicated in asthma.
Liver or Kidney Impairment: Many anti-arrhythmic drugs are metabolized or excreted through the liver or kidneys, so severe hepatic or renal impairment may contraindicate their use or require dose adjustment.
Electrolyte Imbalance: Hypokalemia or hypomagnesemia increases the risk of drug-induced arrhythmias (e.g., torsades de pointes) and should be corrected before using drugs like sotalol, dofetilide, or amiodarone.
Long QT Syndrome: Drugs that prolong QT interval (Class Ia and III) are contraindicated in congenital long QT syndrome or patients with QT-prolonging medications due to risk of torsades de pointes.
Pregnancy and Lactation: Some anti-arrhythmic drugs (e.g., amiodarone) can cross the placenta or appear in breast milk and are contraindicated in pregnancy unless absolutely necessary.
Digitalis Toxicity: Use of digoxin is contraindicated if signs of digitalis toxicity are present (e.g., nausea, confusion, arrhythmia).
It’s crucial for healthcare professionals to carefully consider the specific characteristics of each anti-arrhythmic drug, individual patient factors, and potential contraindications when prescribing these medications. Close monitoring and regular follow-ups are essential to assess the drug’s effectiveness and manage potential side effects. Patients should inform their healthcare providers of any existing medical conditions, medications, or allergies to ensure safe and appropriate use.




