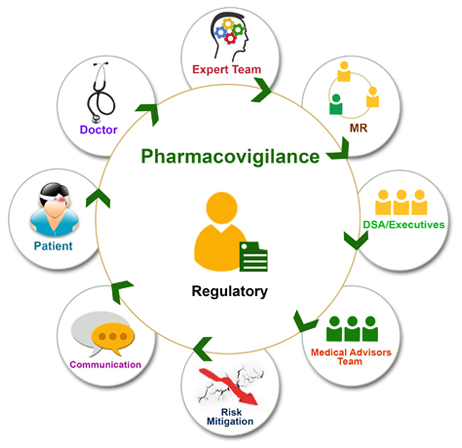
Basic Terminologies in Pharmacovigilance: Pharmacovigilance (PV) is the science and activities related to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problems. Effective pharmacovigilance relies on a well-understood terminology that ensures clarity and accuracy in communication.
1. Basic Terminologies in Pharmacovigilance
1. Pharmacovigilance (PV): Defined by the WHO as “the science and activities relating to the detection, assessment, understanding, and prevention of adverse effects or any other drug-related problems.”
Example: Monitoring adverse effects in post-marketing drug surveillance to ensure safety.
2. Adverse Drug Reaction (ADR): Any noxious, unintended, and undesired effect of a drug that occurs at doses normally used for prophylaxis, diagnosis, therapy, or modification of physiological function.
Example: Anaphylaxis caused by penicillin.
3. Adverse Event (AE): Any untoward medical occurrence in a patient or clinical investigation subject administered a pharmaceutical product, which may or may not be related to the treatment.
Example: A patient develops a rash while on antibiotics, but the rash may or may not be related to the drug.
4. Side Effect: An unintended effect of a drug that occurs at normal therapeutic doses. These can be beneficial or harmful and are often predictable based on the pharmacological action of the drug.
Example: Drowsiness caused by antihistamines like diphenhydramine.
5. Serious Adverse Event (SAE): An adverse event that results in death, is life-threatening, requires hospitalization, causes significant disability or incapacity, or results in a congenital anomaly/birth defect.
Example: Liver failure due to acetaminophen overdose requiring hospitalization.
6. Signal: Information arising from one or multiple sources, such as clinical trials or spontaneous reports, suggesting a new causal association or new aspect of a known association between an intervention and an event.
Example: A signal of cardiotoxicity associated with a new cancer drug based on multiple reports.
7. Benefit-Risk Assessment: The evaluation of the positive therapeutic effects of a drug relative to its adverse effects. This assessment guides regulatory decisions on the approval or withdrawal of drugs.
Example: A cancer drug with a risk of cardiac events may still be approved if the benefit in prolonging life outweighs the risk.
8. Spontaneous Reporting System (SRS): A system where healthcare professionals or consumers report ADRs on their own initiative to regulatory agencies or drug manufacturers.
Example: Reporting an ADR to the FDA’s MedWatch system.
9. Causality Assessment: The process of determining whether a drug is the likely cause of an observed adverse effect. Tools such as the Naranjo Algorithm or WHO Causality Scale are often used.
Example: Determining whether a rash after starting amoxicillin is due to the drug or another cause.
10. Dechallenge and Rechallenge:
Dechallenge: The discontinuation of a drug to see if an ADR resolves.
Rechallenge: The re-administration of the drug to see if the ADR recurs, which can confirm causality.
Example: If a patient’s symptoms disappear after stopping a medication and reappear upon restarting, this suggests the drug was the cause.
11. Risk Management Plan (RMP): A detailed plan developed by pharmaceutical companies to manage the risks associated with a drug. It is required by regulatory agencies before a drug is approved.
Example: The development of an RMP for a new vaccine to monitor rare but serious adverse effects like anaphylaxis.
12. Medication Error: Any preventable event that may lead to inappropriate medication use or patient harm while the medication is in control of the healthcare professional or patient.
Example: Administering the wrong dose of insulin due to a prescribing error.
2. Terminologies of Adverse Medication-Related Events
1. Adverse Drug Event (ADE): Any injury resulting from medical intervention related to a drug, including ADRs and medication errors.
Example: A patient develops renal failure after taking too high a dose of aminoglycosides.
2. Medication Misadventure: Any iatrogenic hazard or incident associated with medications, encompassing both ADEs and medication errors.
Example: A patient mistakenly taking another patient’s prescribed medication.
3. Overdose: The administration of a drug in quantities greater than recommended. It can result in toxic effects or death.
Example: Accidental overdose of opioids leading to respiratory depression.
4. Drug Interaction: When one drug affects the activity of another drug when both are administered together, which may enhance or reduce therapeutic or toxic effects.
Example: Warfarin interacting with certain antibiotics, increasing the risk of bleeding.
5. Allergic Reaction: A hypersensitivity reaction resulting from an immune response to a drug. Can range from mild (rash) to severe (anaphylaxis).
Example: Penicillin-induced anaphylactic shock.
6. Idiosyncratic Reaction: An unusual or unpredictable response to a drug that is not related to the dose or pharmacology.
Example: Malignant hyperthermia triggered by anesthesia in genetically predisposed individuals.
7. Toxicity: The degree to which a substance can cause harm, typically at higher-than-recommended doses.
Example: Acetaminophen toxicity leading to liver damage when taken in excessive amounts.
3. Regulatory Terminologies in Pharmacovigilance
1. Marketing Authorization Holder (MAH): The pharmaceutical company that has been granted permission to market a drug by a regulatory agency.
Example: Pfizer is the MAH for the COVID-19 vaccine Comirnaty.
2. Investigational New Drug (IND): A drug that is being tested in clinical trials and has not yet been approved for general use by a regulatory body.
Example: A new cancer treatment undergoing clinical trials before FDA approval.
3. New Drug Application (NDA): A formal request by a pharmaceutical company to the regulatory agency (e.g., FDA) to approve a new drug for sale and marketing.
Example: Submission of an NDA for a novel anti-diabetic medication.
4. Periodic Safety Update Report (PSUR): A report that provides an evaluation of the benefit-risk balance of a drug, submitted at regular intervals post-marketing.
Example: A PSUR submitted to the European Medicines Agency (EMA) detailing adverse effects from a newly marketed antibiotic.
5. Individual Case Safety Report (ICSR): A report that contains details on a single adverse event or reaction associated with the use of a drug in an individual patient.
Example: A doctor reports an ICSR of a patient experiencing liver failure after taking a statin.
6. Post-Marketing Surveillance (PMS): The monitoring of drugs after they have been approved for use by the regulatory authority. It aims to detect any adverse reactions that were not seen in clinical trials.
Example: Monitoring for adverse effects from a new asthma inhaler after its market launch.
7. Good Pharmacovigilance Practices (GVP): A set of guidelines established by regulatory authorities such as the European Medicines Agency (EMA) to ensure that marketing authorization holders meet their pharmacovigilance obligations.
Example: Companies following GVP guidelines must have robust risk management systems in place.
8. Expedited Reporting: A regulatory requirement to report serious and unexpected adverse drug reactions within a specified timeframe.
Example: A company must report a case of fatal drug-induced hepatitis to the regulatory authority within 15 days.
9. Risk Evaluation and Mitigation Strategy (REMS): A plan required by the FDA to ensure that the benefits of a drug outweigh its risks. REMS may include medication guides, communication plans, or restricted access programs.
Example: A REMS program for isotretinoin (Accutane) to prevent birth defects due to teratogenic effects.
Examples of Regulatory Reporting
1. FDA MedWatch: The FDA’s safety information and adverse event reporting program where healthcare professionals and consumers can report ADRs, product quality issues, and medication errors.
Example: A nurse reports a case of severe rash in a child following administration of a flu vaccine.
2. EudraVigilance (EMA): A system for managing and analyzing information on suspected adverse reactions to medicines authorized or being studied in clinical trials in the European Economic Area.
Example: A pharmaceutical company submits a PSUR for a newly authorized antihypertensive drug to the EMA.
3. Yellow Card Scheme (MHRA, UK): The UK’s system for collecting and monitoring information on suspected ADRs for medicines, vaccines, and medical devices.
Example: A physician reports a case of thrombosis with thrombocytopenia syndrome after a patient received the AstraZeneca COVID-19 vaccine.
Conclusion:
Pharmacovigilance is a critical component of public health and drug safety. The terminology used in PV helps ensure that all stakeholders—regulatory authorities, healthcare professionals, and patients—have a common understanding of adverse drug reactions, regulatory requirements, and post-marketing surveillance activities.
Effective use of these terms enables better detection, reporting, and management of drug-related risks, ultimately safeguarding patient health.

