Blood cells
Red blood cells (RBCs)
Blood cells: Red blood cells, scientifically referred to as erythrocytes, are one of the most essential components of the human circulatory system. These specialized cells are primarily responsible for the transportation of respiratory gases, specifically oxygen and carbon dioxide, between the lungs and various tissues of the body. Produced in the bone marrow through a process called erythropoiesis, red blood cells circulate throughout the bloodstream and serve as a critical link in maintaining cellular respiration and overall metabolic activity in body tissues.
The primary role of red blood cells is to carry oxygen from the alveoli of the lungs to every cell in the body. They achieve this through the action of hemoglobin, a complex iron-containing protein that has the remarkable ability to reversibly bind oxygen. In addition to oxygen transport, erythrocytes also collect carbon dioxide, a byproduct of cellular metabolism, from the tissues and return it to the lungs where it is expelled from the body through exhalation. Thus, red blood cells are central to the processes of gas exchange, acid-base homeostasis, and the maintenance of physiological function.
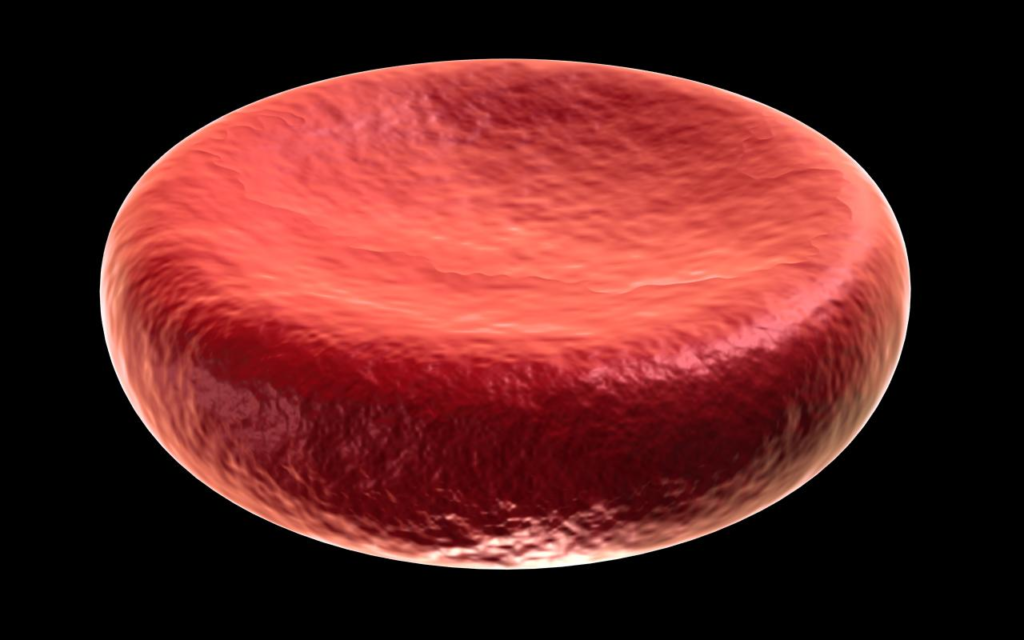
Characteristics of Red Blood Cells
Shape: Human red blood cells possess a distinctive biconcave disc shape, which means they are thinner in the center than at the edges. This unique shape increases the surface area-to-volume ratio, thereby maximizing the efficiency of gas diffusion. Furthermore, mature red blood cells lack a nucleus and other organelles, allowing more internal space for hemoglobin, and making them more flexible to navigate through narrow capillaries.
Color: The red coloration of these cells is attributed to the presence of hemoglobin, which binds with oxygen to form oxyhemoglobin, giving the blood its bright red appearance when oxygenated. Deoxygenated blood appears darker due to the change in the conformation of hemoglobin.
Size and Number: On average, red blood cells measure approximately 6–8 micrometers in diameter. An adult human typically has about 4.5 to 6 million RBCs per microliter of blood, making them the most abundant cell type in the bloodstream.
Lifespan and Turnover: Red blood cells have a lifespan of about 120 days. As they age or become damaged, they are removed from circulation by phagocytic cells in the spleen and liver, organs involved in filtering the blood and recycling iron and other components from the degraded cells.
Functions of Red Blood Cells
Oxygen Transport: The primary function of RBCs is to transport oxygen from the lungs to tissues across the body. Hemoglobin molecules within red blood cells bind oxygen in the pulmonary capillaries and release it in systemic tissues where it is required for aerobic respiration and ATP production.
Carbon Dioxide Transport: Red blood cells also play a crucial role in removing carbon dioxide, a metabolic waste product, from the tissues. This gas is transported in three forms: dissolved in plasma, chemically bound to hemoglobin (as carbaminohemoglobin), and as bicarbonate ions after enzymatic conversion by carbonic anhydrase, an enzyme found in RBCs.
pH Buffering and Homeostasis: Red blood cells help maintain the acid-base balance of the blood by acting as buffers. The carbonic anhydrase enzyme in RBCs facilitates the reversible conversion of carbon dioxide and water to carbonic acid, which dissociates into bicarbonate and hydrogen ions. This system plays a central role in regulating the blood’s pH within a narrow physiological range (~7.35–7.45).
Role in Blood Group Determination: The surface of red blood cells contains antigens that determine an individual’s blood type (e.g., ABO and Rh systems). These antigens are critical in blood transfusions and immune responses.
White blood cells (WBCs)
White blood cells, scientifically known as leukocytes, are a vital component of the human blood and immune system. Unlike red blood cells, which primarily serve in gas transport, white blood cells are specialized immune cells whose main function is to protect the body from infections, foreign substances, and abnormal or cancerous cells. These dynamic cells circulate in the bloodstream and migrate to tissues as needed, where they execute immune surveillance, destroy harmful invaders, and contribute to both innate and adaptive immunity.
WBCs are produced in the bone marrow from multipotent stem cells and are present in significantly lower numbers than red blood cells—typically 4,000 to 11,000 WBCs per microliter of blood. Despite their relatively low number, their impact on human health is enormous, playing a central role in inflammation, immune regulation, tissue repair, and defense mechanisms against a wide array of pathogens such as bacteria, viruses, parasites, and fungi.
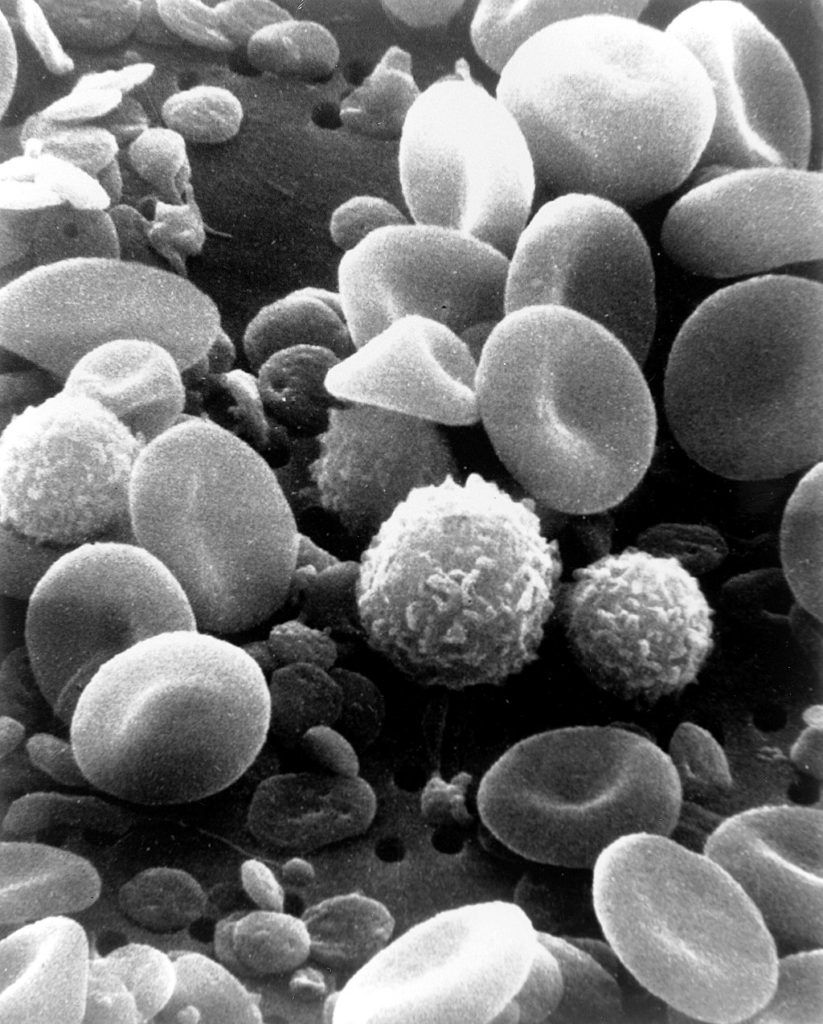
Characteristics of White blood cells
Presence of a Nucleus: Unlike red blood cells, WBCs retain their nucleus and organelles, which allow them to produce proteins and perform complex immune functions.
Size and Appearance: WBCs are generally larger than red blood cells and vary in shape and internal structure, depending on their type. Their nuclei may be segmented (as in neutrophils) or large and round (as in lymphocytes).
Variety and Specialization: White blood cells are not a single cell type, but rather a diverse group of immune cells, each with distinct functions and appearances. The five primary types are:
- Neutrophils
- Lymphocytes (B cells and T cells)
- Monocytes
- Eosinophils
- Basophils
These types are further classified into two major categories:
- Granulocytes (neutrophils, eosinophils, basophils) – characterized by granules in their cytoplasm.
- Agranulocytes (lymphocytes and monocytes) – lacking visible granules.
Functions of White blood cells
1. Immune Defense and Surveillance: The overarching function of WBCs is to detect, attack, and eliminate infectious agents and foreign bodies. They continuously monitor tissues for signs of danger or infection.
2. Phagocytosis: Certain WBCs, such as neutrophils and monocytes, act as phagocytes—they engulf pathogens, damaged cells, or debris and digest them using enzymes. This is one of the body’s first lines of defense in innate immunity.
3. Antibody Production: A subset of WBCs known as B lymphocytes (B cells) produce antibodies, which are specific proteins that bind to antigens on pathogens. These antibodies neutralize invaders or tag them for destruction by other immune cells.
4. Immune Memory and Adaptive Response: After an infection, certain lymphocytes such as Memory B cells and Memory T cells remain in the body, storing information about the pathogen. Upon re-exposure, they trigger a faster and more potent immune response, forming the basis for immunological memory—the principle behind vaccines.
5. Allergic and Inflammatory Responses: Eosinophils and basophils are involved in mediating allergic reactions and inflammation. Basophils release histamine, which contributes to allergic symptoms and inflammation, while eosinophils help combat parasitic infections.
6. Cytotoxic Activity: T lymphocytes, particularly cytotoxic T cells, can directly kill virus-infected or cancerous cells, contributing to immune regulation and tumor surveillance.
Platelets (Thrombocytes)
Platelets, also referred to as thrombocytes, are small, irregularly-shaped cell fragments that circulate in the blood and play a fundamental role in the physiological process known as hemostasis—the stopping of bleeding from damaged blood vessels. Though they lack a nucleus, platelets are metabolically active and possess specialized organelles and granules that are essential for their role in blood clotting and wound healing.
These cell fragments originate from large bone marrow cells called megakaryocytes. When megakaryocytes mature, they shed small portions of their cytoplasm into the bloodstream in the form of platelets. Despite their tiny size and short lifespan, platelets are essential in maintaining vascular integrity, initiating blood clot formation, and facilitating tissue repair after injury.
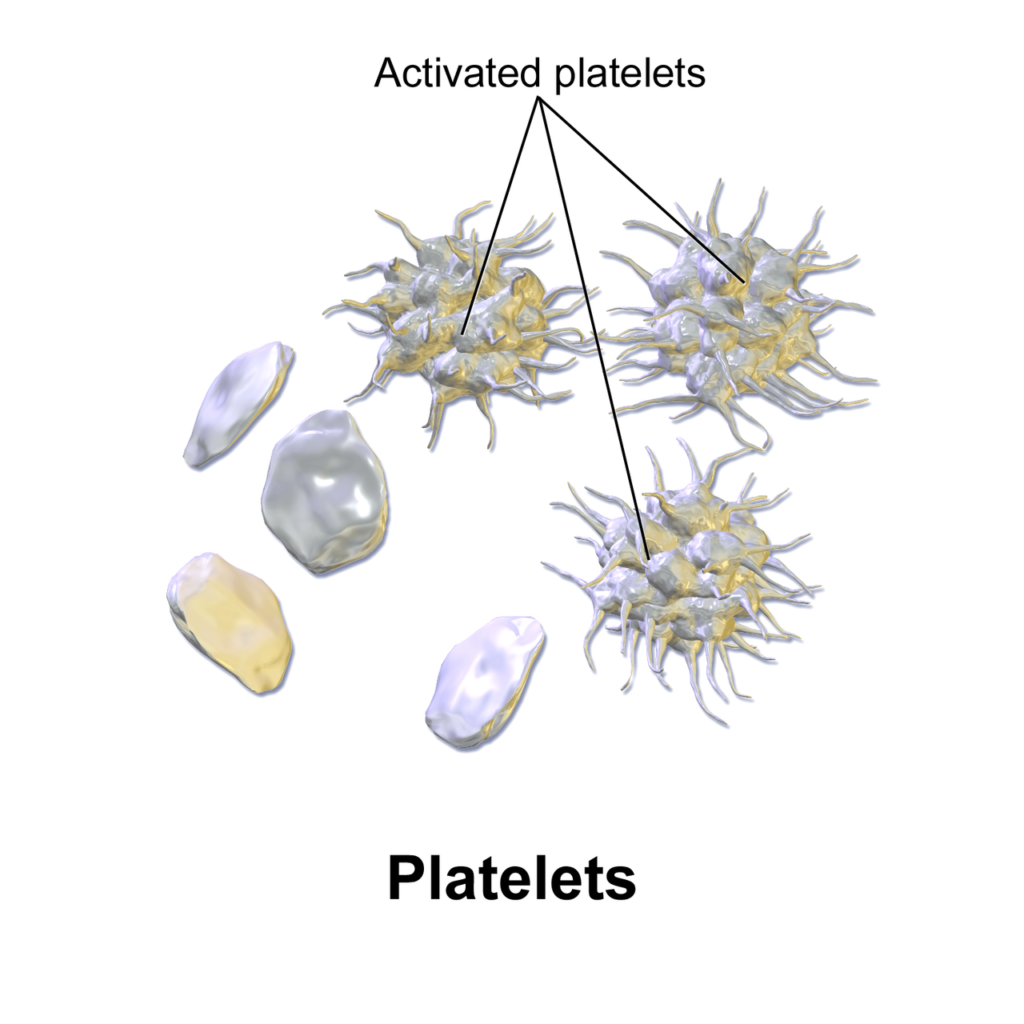
Characteristics of Platelets:
Not Whole Cells: Platelets are cytoplasmic fragments derived from megakaryocytes. They do not contain a nucleus, distinguishing them from most other blood cells.
Size and Shape: They are small, disc-shaped particles, usually measuring about 2–3 micrometers in diameter, which allows them to swiftly navigate through the vascular system.
Colorless and Granulated: Under microscopic observation, platelets appear colorless and possess numerous granules that store enzymes, clotting factors, calcium, and growth factors necessary for their function.
Short Lifespan: Platelets have a relatively brief life in circulation, typically 8 to 10 days, after which they are removed from the bloodstream by the spleen and liver.
Normal Count: A healthy adult usually has 150,000 to 450,000 platelets per microliter of blood. Levels below or above this range may indicate bleeding disorders or thrombotic conditions.
Functions of Platelets
1. Hemostasis (Blood Clotting): The primary function of platelets is to prevent blood loss through a rapid and efficient process known as hemostasis. This involves three major steps:
Adhesion: Upon vascular injury, platelets are attracted to exposed collagen fibers at the damaged endothelium and adhere to the injury site using surface receptors like glycoprotein Ib (GpIb).
Activation: Once adhered, platelets become activated, changing shape (from disc to spiny forms), and releasing chemical mediators such as ADP, thromboxane A₂, serotonin, and calcium ions.
Aggregation: Activated platelets stick together to form a platelet plug, reinforced by fibrin strands that stabilize the clot. This temporary plug effectively halts bleeding.
2. Vasoconstriction: Platelets also contribute to vasoconstriction, the narrowing of blood vessels, by releasing vasoactive substances like serotonin. This reduces blood flow to the affected area, limiting further blood loss and aiding clot stability.
3. Clot Retraction and Repair: Platelets participate in clot retraction, where the formed clot is compacted to reduce its size and bring wound edges closer together. They release growth factors such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-β) that promote tissue regeneration and endothelial repair.
4. Immunological Role: Recent research also highlights the immunomodulatory role of platelets. They can interact with immune cells and release cytokines that influence inflammation and immune responses, acting beyond their traditional role in clotting.
Clinical Relevance:
Thrombocytopenia (low platelet count) can lead to excessive bleeding and bruising.
Thrombocytosis (high platelet count) can increase the risk of abnormal clotting, potentially resulting in stroke, heart attack, or deep vein thrombosis (DVT).
Platelet transfusions are commonly used in medical treatments where patients experience dangerously low platelet levels, such as during chemotherapy or bone marrow disorders.

