Blood groups: In the year 1900, Austrian scientist Karl Landsteiner discovered the ABO blood group system. In his experiments, he mixed different blood types, observing that the plasma from specific blood types produced agglutinates or formed clusters. This phenomenon was caused by the absence of molecules on red blood cells, which, in turn, led to the production of antibodies aimed at countering the missing molecule.
Karl Landsteiner further classified the blood types into four different groups based on the observed agglutination. For his groundbreaking discovery of the ABO blood group system, he was honored with the Nobel Prize.
ABO blood Group system
The ABO blood group system is one of the most fundamental and well-known systems for classifying human blood. It is based on the presence or absence of two antigens, A and B, on the surface of red blood cells (erythrocytes). This system was first discovered and characterized by the Austrian immunologist Karl Landsteiner in the early 20th century and has since played a critical role in blood transfusions and various medical applications. Here’s a detailed overview of the ABO blood group system:
Antigens and Antibodies
The presence or absence of specific antigens on the surface of red blood cells determines ABO blood groups. These antigens consist of carbohydrates (glycoproteins) and are genetically inherited.
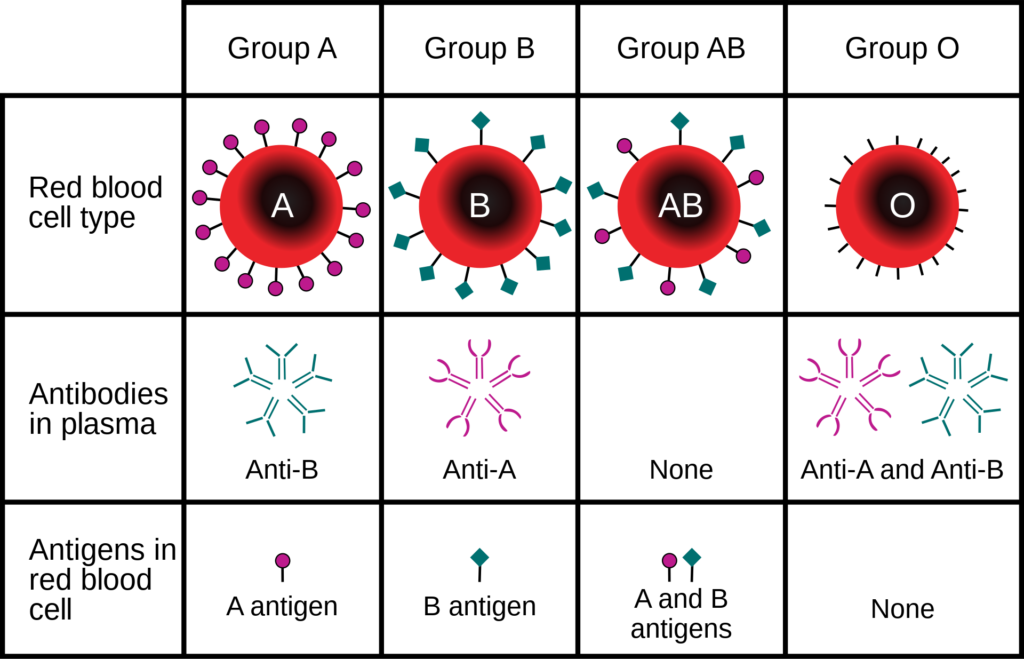
- There are two main antigens in the ABO system:
- A antigen (also known as antigen A)
- B antigen (also known as antigen B)
- In addition to the antigens on red blood cells, individuals also produce antibodies against the antigens they lack:
- Blood type A individuals have anti-B antibodies in their plasma.
- Blood type B individuals have anti-A antibodies in their plasma.
- Blood type AB individuals have neither anti-A nor anti-B antibodies in their plasma.
- Blood type O individuals have both anti-A and anti-B antibodies in their plasma.
Blood Types
There are four primary blood types within the ABO system:
- Blood type A: This blood type has A antigens on the surface of red blood cells and anti-B antibodies in the plasma.
- Blood type B: This blood type has B antigens on the surface of red blood cells and anti-A antibodies in the plasma.
- Blood type AB: This blood type has both A and B antigens on the surface of red blood cells and lacks anti-A or anti-B antibodies in the plasma.
- Blood type O: This blood type has neither A nor B antigens on the surface of red blood cells but contains both anti-A and anti-B antibodies in the plasma.
During blood donation or transfusion, the ABO group system plays a vital role because mismatched blood groups can cause red blood cells to clump and lead to various disorders. It is crucial that the blood cells match between the donor and recipient, ensuring compatibility. For instance, a person with blood group A can receive blood from group A or O since there are no antibodies for A and O in blood group A. People with blood group O are referred to as universal donors, while those with blood group AB are universal recipients.
Rh factor
The Rh blood group system, also known as the Rhesus factor, is an important classification system for categorizing human blood based on the presence or absence of the Rh antigen (D antigen) on the surface of red blood cells (erythrocytes). The Rh system is named after the Rhesus monkey, in which this antigen was first discovered. Here’s a detailed overview of the Rh blood group system:
Rh Antigen (D Antigen)
- The Rh antigen, also called the D antigen, is a protein that is either present (Rh-positive) or absent (Rh-negative) on the surface of red blood cells.
- Rh-positive individuals have the Rh antigen on their red blood cells, while Rh-negative individuals lack this antigen.
- The presence or absence of the Rh antigen is genetically determined and inherited from parents.
Inheritance
- The gene responsible for the Rh factor is located on chromosome 1. This gene has two main alleles: D (for the presence of the Rh antigen) and d (for the absence of the Rh antigen).
- An individual’s Rh status is determined by their genotype, with three possible combinations:
- DD: The individual is Rh-positive and carries two copies of the Rh antigen gene.
- Dd: The individual is Rh-positive and carries one Rh antigen gene and one non-Rh antigen gene.
- dd: The individual is Rh-negative and lacks the Rh antigen gene.
Importance of Rh Factors
- The Rh factor is crucial in various medical and clinical situations:
- Blood Transfusions: Rh compatibility is considered in blood transfusions. Rh-negative individuals can generally receive Rh-negative or Rh-positive blood, while Rh-positive individuals should receive Rh-positive blood. Mixing Rh-positive blood with Rh-negative blood can lead to sensitization and potential adverse reactions.
- Pregnancy: Rh incompatibility between a Rh-negative mother and a Rh-positive fetus can lead to a condition called Hemolytic Disease of the Newborn (HDN). This occurs when the mother’s immune system produces antibodies against the Rh antigen of the fetus’s blood. To prevent HDN, Rh-negative pregnant women often receive Rh immunoglobulin (RhIg) injections.
- Organ Transplants: Rh compatibility may be considered in organ transplantation to reduce the risk of graft rejection.
Rh Factor in Blood Donations
- Blood banks test for both ABO blood group and Rh factor to determine an individual’s complete blood type. Common blood type designations
- Blood banks conduct tests for both ABO blood group and Rh factor to establish an individual’s complete blood type. Common blood type designations encompass A+, B-, AB+, O-, and more.
- O-negative (O-) individuals often earn the moniker of universal donors because their blood can be safely transfused into individuals with any Rh factor, rendering them crucial in emergency situations.
- AB-positive (AB+) individuals garner recognition as universal recipients since they can receive blood from donors with any Rh factor.

