Calcitonin is a 32-amino acid polypeptide hormone primarily involved in calcium and phosphate homeostasis. It is secreted by the parafollicular C cells of the thyroid gland in mammals and serves as a physiological antagonist to parathyroid hormone (PTH). While its role in human calcium metabolism is less dominant compared to PTH and vitamin D, calcitonin still plays a crucial part in specific physiological and pathological states. Moreover, synthetic and recombinant forms of calcitonin have clinical significance, particularly in managing bone-related disorders.
Structure and Biosynthesis of Calcitonin
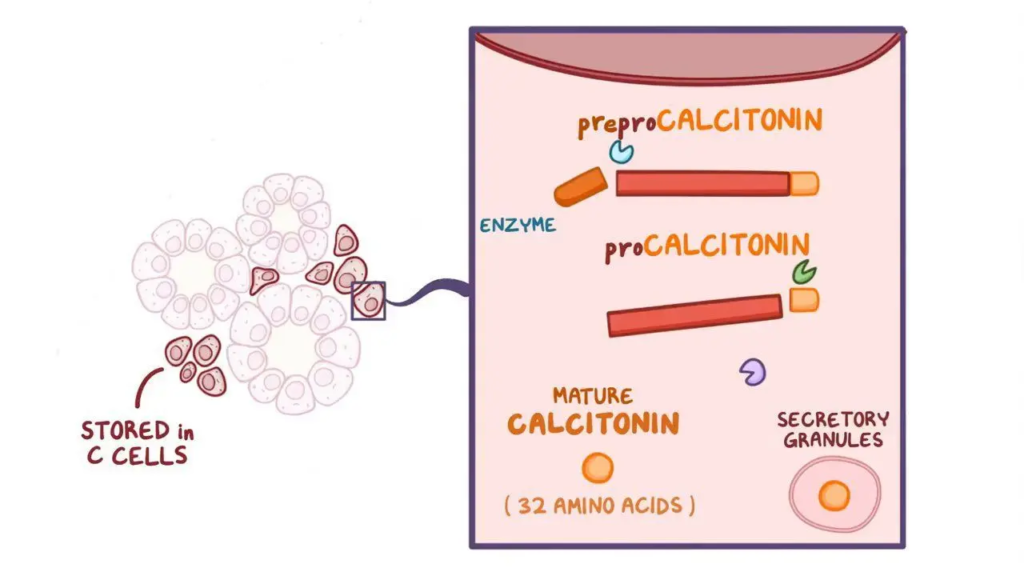
Calcitonin is a linear polypeptide with a molecular weight of about 3.4 kDa. It is synthesized as a preprohormone (preprocalcitonin), which is cleaved in the endoplasmic reticulum and Golgi apparatus to form the biologically active form. The gene encoding calcitonin (CALC1) is located on chromosome 11 and undergoes alternative splicing to produce either calcitonin or calcitonin gene-related peptide (CGRP), a neuropeptide with vasodilatory functions.
Regulation of Secretion of calcitonin
Calcitonin secretion is regulated primarily by:
Plasma Calcium Levels: A rise in serum calcium concentration is the most potent stimulus for calcitonin secretion. This is mediated by calcium-sensing receptors (CaSR) on C cells.
Gastrointestinal Hormones: Gastrin, pentagastrin, and other GI hormones can stimulate calcitonin release.
Beta-Adrenergic Agonists: Sympathetic stimulation may also enhance calcitonin secretion.
Negative feedback by decreased serum calcium levels suppresses calcitonin secretion.
Mechanism of Action of Calcitonin
Calcitonin exerts its effects through the calcitonin receptor (CTR), a G protein-coupled receptor predominantly expressed in:
- Osteoclasts (bone-resorbing cells)
- Renal tubules
- Brain and other peripheral tissues
Upon binding to CTR, calcitonin activates the cAMP pathway and phospholipase C, leading to:
- Inhibition of osteoclastic bone resorption
- Enhanced renal excretion of calcium and phosphate
These effects ultimately contribute to a reduction in serum calcium levels.
Physiological Functions of Calcitonin
1. Paget’s Disease of Bone: Calcitonin is used to manage Paget’s disease, a chronic disorder characterized by abnormal bone remodeling. It helps reduce bone pain and normalize bone turnover by inhibiting osteoclastic activity.
2. Postmenopausal Osteoporosis: Calcitonin is used in postmenopausal women to reduce the rate of bone loss and alleviate bone pain, particularly in vertebral fractures. It is an alternative for patients who cannot tolerate bisphosphonates.
3. Hypercalcemia of Malignancy: Calcitonin provides rapid but short-term control of hypercalcemia, especially when caused by cancer. It reduces serum calcium levels by inhibiting bone resorption and enhancing renal calcium excretion.
4. Bone Pain Due to Osteolytic Metastases: In patients with metastatic bone disease, calcitonin can provide analgesic relief by reducing osteolytic activity and modulating central pain pathways.
5. Reflex Sympathetic Dystrophy (Complex Regional Pain Syndrome): Calcitonin has been used off-label in the treatment of CRPS, where it helps reduce pain and inflammation, particularly in early stages of the disease.
6. Phantom Limb Pain: Intravenous calcitonin has shown some efficacy in reducing phantom limb pain following amputation, possibly through its central analgesic effects.
7. Osteoporosis Associated with Immobilization: In patients who are immobilized due to injury or neurological conditions (e.g., spinal cord injury), calcitonin may help prevent rapid bone loss.
8. Pain Management in Acute Vertebral Compression Fractures: Calcitonin has been used for short-term pain relief in patients with acute vertebral fractures, commonly due to osteoporosis.
Pathophysiology of Calcitonin
1. Source and Secretion: Calcitonin is a peptide hormone secreted by the parafollicular cells (C cells) of the thyroid gland. Its secretion is primarily stimulated by high serum calcium levels (hypercalcemia). Other factors such as certain gastrointestinal hormones (e.g., gastrin) can also stimulate its release, especially after a meal.
2. Role in Calcium Homeostasis: Calcitonin plays a regulatory role in calcium metabolism. Its main function is to lower elevated blood calcium levels. It acts in opposition to parathyroid hormone (PTH), which increases calcium levels. However, in humans, calcitonin has a relatively minor role in normal calcium homeostasis compared to PTH and vitamin D.
3. Action on Bone: The primary target of calcitonin is bone, specifically osteoclasts. Calcitonin binds to receptors on osteoclasts and inhibits their activity, thereby reducing bone resorption. This prevents the release of calcium and phosphate from bone into the bloodstream. As a result, it helps to decrease serum calcium levels.
4. Action on Kidneys: Calcitonin also acts on the renal tubules of the kidneys. It reduces the reabsorption of calcium and phosphate, leading to increased urinary excretion of both. This contributes further to the lowering of serum calcium levels. However, the renal effects are less significant than the effects on bone.
5. Effect on Gastrointestinal Tract: Calcitonin has minimal direct effect on the intestines. However, by lowering blood calcium, it may indirectly reduce the synthesis of calcitriol (active vitamin D), which in turn decreases intestinal absorption of calcium. This effect is secondary and not its main mechanism.
6. Regulation and Feedback Mechanism: Calcitonin secretion is regulated through a negative feedback loop. When blood calcium levels are high, calcitonin is released. As serum calcium returns to normal, calcitonin secretion is reduced. It serves as a short-term regulator of calcium, especially after meals or during acute calcium elevations.
7. Comparison with Parathyroid Hormone (PTH): While PTH increases blood calcium by stimulating bone resorption, increasing intestinal absorption, and promoting renal calcium reabsorption, calcitonin decreases blood calcium by inhibiting bone resorption and increasing renal excretion. Together, they help maintain calcium balance in the body.
8. Clinical Relevance: Although calcitonin has a minor physiological role in adults, it becomes more significant in certain conditions like childhood, pregnancy, and high-calcium states. Pharmacologically, synthetic or salmon-derived calcitonin (which is more potent) is used in the treatment of osteoporosis, Paget’s disease, hypercalcemia, and bone pain.
Therapeutic Uses of Calcitonin
Calcitonin is used clinically for its ability to inhibit bone resorption and regulate calcium metabolism. Synthetic and salmon-derived calcitonin (more potent than human calcitonin) are used in the treatment of various bone and calcium-related disorders. Its therapeutic benefits are primarily due to its anti-resorptive and analgesic properties.
i. Postmenopausal Osteoporosis: Calcitonin is used as an alternative therapy for women with postmenopausal osteoporosis who cannot tolerate or are not candidates for other treatments like bisphosphonates. It helps reduce the rate of vertebral bone loss and provides relief from acute pain following vertebral fractures.
ii. Paget’s Disease of Bone: In patients with Paget’s disease, calcitonin helps reduce abnormal bone turnover by inhibiting osteoclastic activity. It provides symptomatic relief from bone pain and helps normalize serum alkaline phosphatase levels, a marker of disease activity.
iii. Hypercalcemia of Malignancy: Calcitonin is used for the short-term management of hypercalcemia, especially when associated with malignancies. It acts rapidly to lower serum calcium levels by decreasing bone resorption and increasing renal calcium excretion. Though the effect is transient, it is useful in acute settings alongside other therapies.
iv. Bone Pain Due to Osteolytic Metastases: Calcitonin may provide palliative relief in patients suffering from bone pain caused by osteolytic lesions due to metastatic cancers. Its analgesic effects are particularly beneficial in managing cancer-related skeletal complications.
v. Reflex Sympathetic Dystrophy (Complex Regional Pain Syndrome): Calcitonin has been used off-label in cases of CRPS to reduce pain and improve mobility. Its exact mechanism in this condition is not fully understood, but it may involve central modulation of pain pathways.
vi. Phantom Limb Pain: Intravenous or intranasal calcitonin has shown efficacy in reducing phantom limb pain in amputees. The hormone appears to influence central pain processing, making it useful in neuropathic pain syndromes.
vii. Acute Vertebral Fracture Pain: Calcitonin is beneficial for the short-term management of acute pain following osteoporotic vertebral fractures. It is particularly useful in the early stages of recovery when pain is severe.
viii. Immobilization-Induced Hypercalcemia or Bone Loss: Patients who are immobilized for long periods (e.g., spinal cord injuries, prolonged bed rest) may develop hypercalcemia or rapid bone loss. Calcitonin can help counteract these effects by suppressing osteoclastic bone resorption.
Pharmacokinetics and Dosage
Formulations:
Salmon calcitonin (more potent, longer half-life)
Human calcitonin (less commonly used)
Routes of Administration:
Nasal spray (200 IU per day)
Subcutaneous or intramuscular injections (100 IU per day)
Intravenous infusions (in acute hypercalcemia)
Metabolism and Excretion:
Calcitonin is degraded in the kidney, liver, and blood.
Has a plasma half-life of about 10–15 minutes (longer with salmon calcitonin).
Adverse Effects
Common Side Effects: Nausea, Facial flushing, Injection site reactions, Nasal irritation (with intranasal form)
Rare and Serious Effects: Hypocalcemia, Allergic reactions (especially with salmon calcitonin), Development of neutralizing antibodies (reducing long-term efficacy)
Limitations and Decline in Use
While calcitonin was widely used in the past, its clinical use has declined due to:
- Development of resistance (tachyphylaxis)
- Emergence of more effective agents such as bisphosphonates and denosumab
- Concerns over carcinogenic potential with long-term use (noted in some animal studies)
- Regulatory agencies like the EMA and FDA have issued warnings or limited indications for calcitonin.
Future Directions and Research
Calcitonin Gene-Related Peptide (CGRP) Pathway: CGRP, encoded by the same gene as calcitonin, is being targeted in migraine therapy. Calcitonin receptor-like receptor (CRLR) and its modulators may become therapeutic targets in cardiovascular and pain conditions.
Novel Analogs and Delivery Systems: Research is ongoing to develop oral, transdermal, and long-acting formulations of calcitonin. Nanocarrier delivery systems may overcome bioavailability issues.
Bone Regeneration and Tissue Engineering: Potential use in orthopedic and dental implants to promote bone healing. Combination therapies with stem cells and growth factors are under exploration.
Conclusion
Calcitonin, though a relatively minor player in human calcium homeostasis compared to PTH and vitamin D, remains a molecule of great biological and clinical interest. Its roles in bone metabolism, renal calcium handling, and pain modulation, along with its diagnostic significance in medullary thyroid carcinoma, make it an important tool in both endocrinology and oncology.
Despite its decreasing role in the treatment of osteoporosis and Paget’s disease due to more potent alternatives, calcitonin continues to have niche applications in acute hypercalcemia and bone pain management. Moreover, research into CGRP and calcitonin analogs promises new avenues for therapy in neurology and beyond.