Cardiac output and the cardiac cycle are fundamental concepts in cardiovascular physiology, describing how the heart functions to pump blood throughout the body. Understanding these processes is crucial for assessing heart health and overall circulatory function. Here’s a detailed note on cardiac output and the cardiac cycle:
Cardiac Output (CO)
Cardiac output is the volume of blood pumped by the heart per minute, usually measured in milliliters or liters per minute (mL/min or L/min).
It is a key indicator of how effectively the heart is performing its pumping function and how well it is meeting the body’s oxygen and nutrient demands.
Calculation of Cardiac Output:
CO = Heart Rate (HR) x Stroke Volume (SV)
Heart Rate (HR): The number of heartbeats per minute, typically ranging from 60 to 100 beats per minute in a resting adult.
Stroke Volume (SV): The amount of blood pumped by the left ventricle with each heartbeat. It is usually around 70 mL per beat in a resting adult.
Cardiac Cycle
The cardiac cycle refers to the sequence of events that occur during one complete heartbeat. It is divided into two phases:
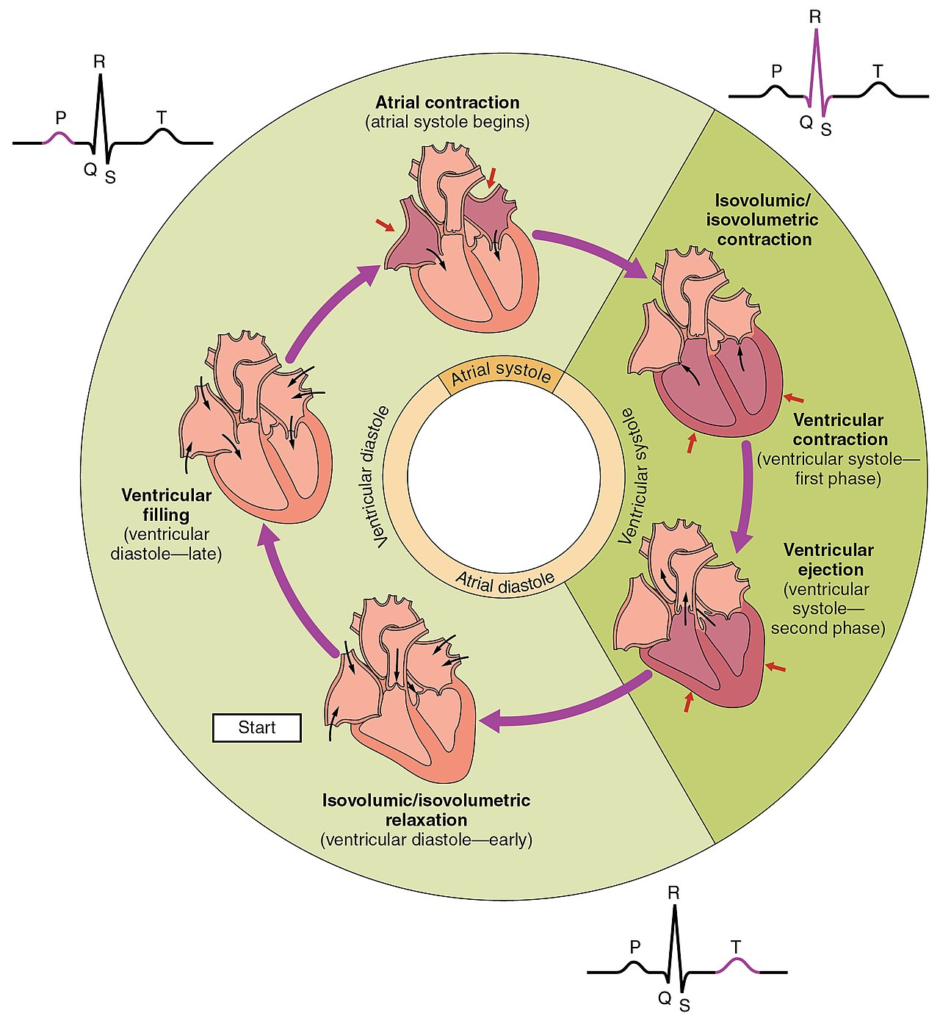
1. Systole
Systole is the phase of the cardiac cycle during which the heart contracts and pumps blood into the arteries. It is further divided into atrial systole (contraction of the atria) and ventricular systole (contraction of the ventricles). During atrial systole, the atria contract to push blood into the ventricles. Ventricular systole involves the contraction of the ventricles, which forces blood into the pulmonary artery and aorta.
2. Diastole
Diastole is the phase during which the heart relaxes and refills with blood. Atrial diastole occurs when the atria relax, allowing them to fill with blood from the venous circulation. Ventricular diastole takes place as the ventricles relax, enabling blood to flow into them from the atria.
Cardiac Cycle Events
The cardiac cycle refers to the sequence of mechanical and electrical events that occur during one complete heartbeat. It includes alternating phases of contraction (systole) and relaxation (diastole) of the atria and ventricles. The events ensure the proper movement of blood through the heart and into the systemic and pulmonary circulations. Below is a detailed description of each phase:
1. Atrial Contraction (Atrial Systole): This phase begins when the sinoatrial (SA) node, known as the natural pacemaker of the heart, generates an electrical impulse. This impulse rapidly spreads across the walls of both the right and left atria, stimulating the atrial muscle fibers to contract. As a result, the blood present in the atria is actively pushed into the relaxed ventricles, topping off the ventricular volume.
During this stage, the atrioventricular (AV) valves — namely the tricuspid valve on the right side and the mitral (bicuspid) valve on the left — are open, allowing smooth blood flow into the ventricles. The semilunar valves (pulmonary and aortic valves) remain closed at this point. This phase contributes approximately the final 20–30% of ventricular filling.
2. Ventricular Contraction (Ventricular Systole): After the ventricles are adequately filled with blood, the electrical impulse travels from the AV node down the bundle of His, and then through the right and left bundle branches and the Purkinje fibers, which distribute the impulse throughout the ventricular myocardium.
This results in ventricular contraction, increasing the pressure within the ventricles. Once the intraventricular pressure exceeds the pressure in the atria, the AV valves close, producing the first heart sound (S1) or the “lub” sound. As the pressure continues to rise, it surpasses the pressure in the pulmonary artery and the aorta, causing the semilunar valves to open.
Blood is then forcefully ejected from the right ventricle into the pulmonary artery (toward the lungs) and from the left ventricle into the aorta (toward the rest of the body). This phase is critical for ensuring effective circulation of oxygenated and deoxygenated blood.
3. Isovolumetric Relaxation: Once the ventricles have ejected most of their blood, they begin to relax, initiating the early part of ventricular diastole. During this short period, all four heart valves remain closed, and no blood enters or leaves the heart chambers.
This phase is termed isovolumetric relaxation because the volume of blood in the ventricles remains unchanged, while the ventricular muscles are relaxing and the pressure inside the ventricles is falling. The closure of the semilunar valves (aortic and pulmonary) due to backflow of blood causes the second heart sound (S2) or the “dub” sound.
The atria are simultaneously filling with blood during this phase, preparing for the next cycle.
4. Atrial Filling: As ventricular pressure continues to drop below the pressure in the atria, the AV valves reopen, marking the start of passive ventricular filling. Blood that has been returning to the atria from the systemic and pulmonary veins now flows passively into the ventricles, driven by the pressure gradient.
This filling phase occurs without atrial contraction and accounts for about 70–80% of ventricular filling. Meanwhile, the atria continue to fill with blood from the superior and inferior vena cava (into the right atrium) and the pulmonary veins (into the left atrium). This phase prepares the heart chambers for the next atrial contraction, thus completing the cardiac cycle.
| Phase | Event Description |
|---|---|
| Atrial Systole | Atria contract; blood moves into relaxed ventricles |
| Ventricular Systole | Ventricles contract; AV valves close; semilunar valves open; blood is ejected |
| Isovolumetric Relaxation | Ventricles relax; all valves are closed; pressure drops |
| Passive Filling | AV valves open; blood flows passively into ventricles from atria |
Significance of the Cardiac Cycle and Cardiac Output
The cardiac cycle ensures that blood is continuously circulated throughout the body, supplying oxygen and nutrients and removing waste products.
Cardiac output reflects the heart’s ability to meet the body’s metabolic demands and maintain tissue perfusion.
Various factors, including heart rate, stroke volume, and the autonomic nervous system, influence cardiac output.

