The Defined Daily Dose (DDD) is an internationally recognized statistical unit developed by the World Health Organization (WHO) through its Collaborating Centre for Drug Statistics Methodology. It represents the assumed average maintenance dose per day for a drug when used for its principal indication in adult populations. This standardized metric facilitates meaningful comparisons of drug utilization across diverse healthcare systems, geographical regions, and time periods, irrespective of variations in pricing, strength, or prescription practices.
1. Purpose and Significance of the Defined Daily Dose (DDD)
The primary objectives of establishing DDDs are to:
- Standardize drug usage data: DDDs provide a uniform denominator for comparing the consumption of different drugs, even across varied dosage forms and therapeutic regimens.
- Enable cross-national and regional comparisons: DDD acts as a global reference tool, aiding in international surveillance and policy-making on medication use.
- Monitor longitudinal trends: It is indispensable in observing the trajectory of drug consumption over time, facilitating early detection of irrational drug use or shifts in prescribing behavior.
- Enhance public health decision-making: Through its quantifiable nature, DDD informs regulatory bodies and health ministries in forming evidence-based drug policies and interventions.
2. Determination of DDD by WHO
The WHO assigns a DDD to a drug based on:
- The average daily dose most frequently prescribed for the main therapeutic indication in adults.
- Clinical evidence regarding the dose required to achieve the intended therapeutic effect.
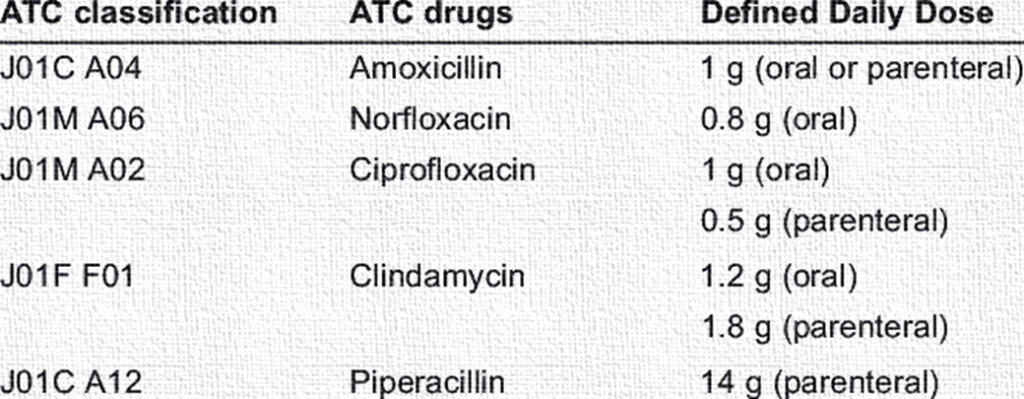
Examples:
- Paracetamol (Acetaminophen): DDD = 3 grams/day (used primarily for pain and fever).
- Metformin: DDD = 2 grams/day (used in Type 2 diabetes mellitus).
It’s crucial to note that the DDD is a technical unit and may not reflect the prescribed daily dose (PDD) or the dose actually consumed by patients.
3. Applications of DDD in Health Systems
a) Drug Utilization Research
DDD is a cornerstone in pharmacoepidemiology and is routinely used in:
- Evaluating public health strategies aimed at reducing overuse or misuse of medications (e.g., antibiotics, benzodiazepines).
- Mapping prescribing patterns across different levels of healthcare—primary care, tertiary hospitals, or private practice.
b) Drug Consumption Surveillance
- Antibiotic monitoring: DDD metrics are pivotal in detecting excessive or inappropriate antimicrobial use—an important factor in combating antimicrobial resistance (AMR).
- Measuring access to essential medicines: Particularly in low-resource settings, DDD data can reflect the penetration of essential drugs within communities.
c) Pharmacoeconomic Analysis
- DDD aids in cost-analysis models, helping to compare the cost-effectiveness and budget impact of different therapeutic regimens across populations and healthcare settings.
4. Calculation and Expression of DDD
Drug consumption is typically expressed as:
- DDD per 1,000 inhabitants per day: Ideal for population-level assessments.
- DDD per 100 bed-days: Used in institutional (hospital-based) studies.
Calculation Example:
A drug with a DDD of 100 mg is consumed at a total quantity of 100,000 mg by a population of 10,000.
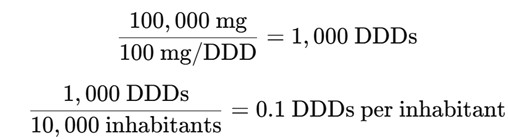
This can be extrapolated to reflect daily usage rates across populations.
5. Advantages and Limitations of the DDD System
Advantages:
- Global Standardization: Enables comparisons across countries, institutions, and timeframes.
- Simplicity & Clarity: Reduces complex pharmacological data into accessible, interpretable figures.
- Versatility: Useful in pharmacovigilance, policy-making, academic research, and hospital audits.
Limitations:
- Lack of individualization: DDD does not account for variability in prescribed dosages, especially in pediatric, geriatric, or renal-compromised populations.
- Not indicative of actual use: It may overestimate or underestimate real drug consumption due to differences in clinical practice.
- Unsuitable for multi-drug therapies: DDD cannot effectively capture polypharmacy patterns or synergistic regimens.
6. Common Public Health Applications
- Antibiotic Stewardship Programs: DDD tracking helps assess and promote rational antibiotic use.
- Chronic Disease Surveillance: Monitoring the use of medications such as statins, antihypertensives, and oral hypoglycemics.
- Global Benchmarking: WHO and other international bodies use DDD-based metrics to compare drug use across countries, promoting harmonized healthcare standards.
Conclusion
The Defined Daily Dose (DDD) serves as an essential epidemiological and pharmacological tool that provides clarity, consistency, and comparability in the realm of drug utilization studies. By offering a standardized methodology, it enables healthcare professionals, researchers, and policymakers to identify trends, ensure rational medication use, evaluate therapeutic accessibility, and implement impactful public health strategies. While not devoid of limitations, DDD continues to be a pivotal measure in understanding global drug consumption patterns and shaping responsible pharmaceutical practices.

