Gout is a form of inflammatory arthritis characterized by the accumulation of uric acid crystals in the joints, causing sudden and severe pain, redness, swelling, and tenderness. It is often referred to as “the disease of kings” due to its historical association with indulgent lifestyles and the consumption of rich foods and alcohol.
Epidemiology of Gout
Gout is one of the most common forms of inflammatory arthritis, affecting approximately 4% of adults in Western countries. It predominantly affects men, with the incidence increasing with age, especially after the age of 30. Women are generally less affected until menopause, after which the prevalence in women rises significantly. The disease is more common in individuals with obesity, metabolic syndrome, and kidney disease. Gout prevalence has been rising globally, particularly due to increasing rates of obesity and lifestyle-related factors.
Etiology of Gout
The primary cause of gout is hyperuricemia, which is an elevated level of uric acid in the blood. Uric acid is the end product of purine metabolism, which is a normal breakdown product of food, especially from meat, seafood, and alcoholic beverages. Hyperuricemia leads to the formation of urate crystals in the joints, triggering an inflammatory response. The major etiological factors include:
1. Hyperuricemia: Increased production of uric acid: Conditions such as overproduction of purines from excessive cell turnover (e.g., leukemia, psoriasis) or high dietary intake.
Decreased excretion of uric acid: Impaired kidney function or dehydration can reduce uric acid excretion through the urine, leading to its accumulation.
2. Dietary Factors: High intake of purine-rich foods (red meats, shellfish, organ meats). Excessive alcohol consumption, particularly beer and spirits, which increases uric acid production.
3. Genetic Factors: Genetic predisposition plays a significant role in gout, with some individuals having a family history of the disease.
4. Comorbidities: Conditions like obesity, hypertension, diabetes, and kidney disease increase the risk of gout by contributing to hyperuricemia.
5. Medications: Diuretics, aspirin, and certain immunosuppressants can increase the risk of gout by affecting uric acid excretion.
6. Trauma or Surgery: Physical stress on the body, such as after trauma or surgery, can precipitate a gout attack by triggering the release of uric acid into the bloodstream.
Pathophysiology of Gout
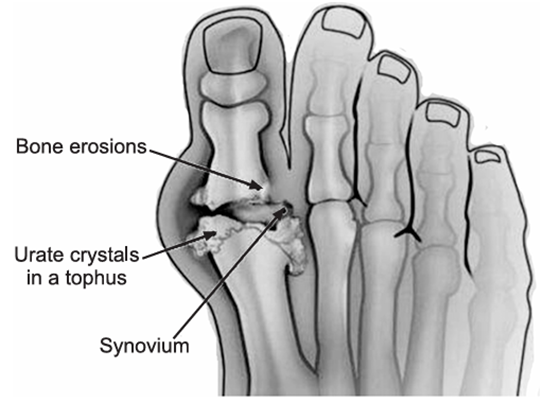
Gout occurs when uric acid, a byproduct of purine metabolism, accumulates in the blood at levels higher than normal (hyperuricemia). When the concentration of uric acid exceeds the solubility limit, it forms monosodium urate crystals, which deposit in the joints, tendons, and surrounding tissues.
The following steps describe the pathophysiology:
1. Crystal Formation: When the level of uric acid in the blood becomes too high, monosodium urate crystals form. These crystals are needle-like in shape and can be deposited in the synovial fluid of joints, especially in cooler areas of the body such as the toes and feet.
2. Inflammatory Response: The urate crystals are recognized by the immune system, triggering an inflammatory response. White blood cells (neutrophils) are recruited to the affected joint, where they attempt to engulf the crystals. This process leads to the release of pro-inflammatory cytokines and enzymes, causing swelling, pain, and redness typical of a gout flare.
3. Chronic Gout: If left untreated, repeated episodes of crystal deposition and inflammation can lead to chronic gout, resulting in joint damage, tophi (large deposits of uric acid crystals under the skin), and kidney stones.
Symptoms of Gout
The classic presentation of gout includes:
1. Acute Gout Attack: Gout typically presents with sudden, severe pain, often starting in the big toe (podagra), but it can also affect the ankles, knees, wrists, or elbows. The affected joint becomes red, warm, and swollen, with intense pain that usually worsens at night. There is also a limited range of motion in the affected joint.
2. Chronic Gout: Gout is characterized by recurrent episodes of joint pain and inflammation. Over time, tophi, which are visible lumps caused by long-term urate crystal deposits, may develop in areas like the fingers, ears, and around joints. In severe, untreated cases, joint deformities and damage can occur.
3. Kidney Involvement: Formation of uric acid crystals in the kidneys may lead to kidney stones, causing pain, hematuria, and impaired renal function.
Tests and Diagnosis of Gout
The diagnosis of gout is based on clinical presentation, laboratory tests, and imaging studies.
1. Clinical Presentation: A history of sudden, severe pain in a single joint, especially the big toe, combined with characteristic signs of inflammation (redness, swelling, warmth).
2. Laboratory Tests:
Serum Uric Acid Levels: Hyperuricemia (elevated levels of uric acid) supports the diagnosis, though some patients with gout may not have elevated levels during an acute attack.
Synovial Fluid Analysis: The gold standard for diagnosing gout is the identification of monosodium urate crystals in the synovial fluid aspirated from the affected joint. The crystals appear as needle-shaped, negatively birefringent under polarized light.
Complete Blood Count (CBC): Often shows elevated white blood cell count due to inflammation.
3. Imaging Studies:
X-rays: May show signs of joint damage and tophi in chronic gout, though they are not useful for diagnosing acute gout attacks.
Ultrasound: Can identify urate crystals in the joints and soft tissues.
Dual-Energy CT (DECT): A more advanced imaging technique that can visualize urate crystal deposits in joints and soft tissues.
Treatments and Drugs of Gout
The management of gout involves both acute treatment of flare-ups and long-term strategies to prevent further attacks and complications.
Acute Treatment:
The goal of acute treatment is to reduce pain and inflammation during a flare-up:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Commonly used to relieve pain and inflammation during a gout attack. Examples include ibuprofen and naproxen.
2. Colchicine: A drug that reduces the inflammatory response caused by urate crystals. It is most effective when taken early in the course of an acute attack.
3. Corticosteroids: Oral or intra-articular corticosteroids (e.g., prednisone) may be used in patients who cannot tolerate NSAIDs or colchicine.
Long-Term Management:
The goal of long-term treatment is to lower uric acid levels and prevent future attacks of gout.
1. Urate-Lowering Therapy (ULT):
Allopurinol: The most commonly prescribed drug for lowering uric acid levels. It inhibits the enzyme xanthine oxidase, which is responsible for uric acid production.
Febuxostat: Another xanthine oxidase inhibitor that lowers uric acid levels in patients who cannot tolerate allopurinol.
Probenecid: A uricosuric drug that increases the excretion of uric acid through the kidneys.
Pegloticase: An enzyme that breaks down uric acid, used in severe cases of gout or those unresponsive to other treatments.
2. Lifestyle Modifications:
Diet: Reducing intake of purine-rich foods (red meats, organ meats, shellfish) and alcohol, particularly beer, can help prevent gout attacks.
Weight Loss: Losing excess weight can reduce uric acid levels and decrease the risk of gout flare-ups.
Hydration: Staying well-hydrated helps prevent uric acid crystal formation in the kidneys and joints.
Pain Management:
In addition to NSAIDs and colchicine, pain relief can be achieved with acetaminophen or corticosteroids in cases where inflammation is severe and other treatments are not appropriate.
Gout is a painful form of arthritis that is caused by the deposition of uric acid crystals in the joints. It can be managed effectively with acute medications such as NSAIDs, colchicine, and corticosteroids, and long-term therapies to lower uric acid levels, such as allopurinol, febuxostat, and lifestyle changes. Early diagnosis and treatment are important to prevent chronic gout and complications such as joint damage and kidney stones.
Visit to: Pharmacareerinsider.com

