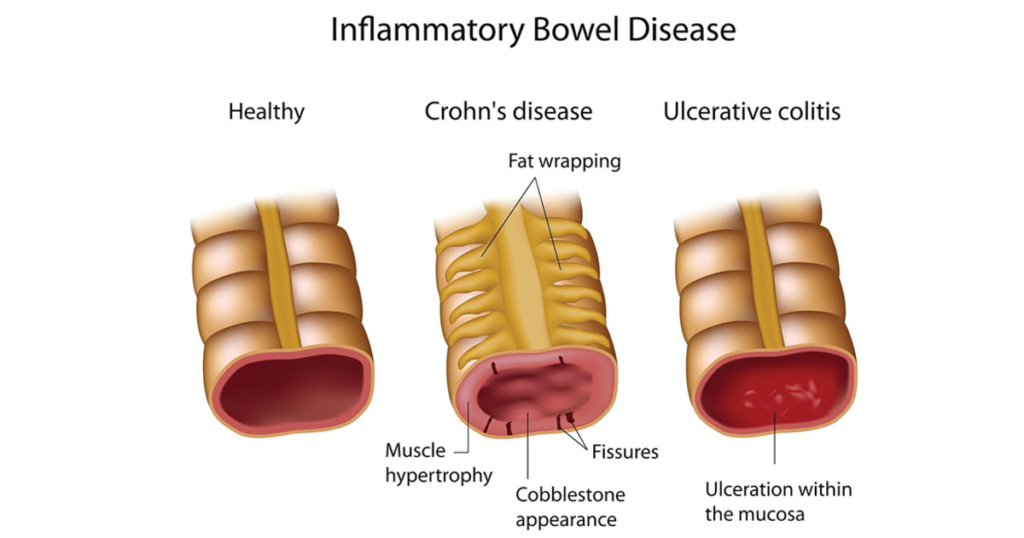
Inflammatory Bowel Diseases (IBD) are chronic inflammatory conditions of the gastrointestinal (GI) tract that primarily include Crohn’s disease (CD) and ulcerative colitis (UC). Both conditions are marked by periods of remission and flare-ups, significantly impacting patients’ quality of life. While the exact cause is unknown, IBD is thought to arise from an interplay of genetic, environmental, microbial, and immune factors.
Epidemiology of Inflammatory Bowel Diseases
Prevalence: IBD affects millions globally, with higher incidence rates in developed countries, particularly in North America, Europe, and urbanized regions of Asia.
Age of Onset: Most commonly diagnosed between ages 15-35, with a smaller peak in later adulthood.
Gender: Ulcerative colitis shows a slight male predominance, while Crohn’s disease has a slightly higher prevalence in females.
Types of of Inflammatory Bowel Diseases
1. Crohn’s Disease (CD)
Crohn’s Disease can affect any part of the gastrointestinal (GI) tract, ranging from the mouth to the anus, with the terminal ileum and colon being the most commonly involved sites. The inflammation in Crohn’s Disease is transmural, meaning it extends through the entire thickness of the bowel wall, and is characterized by skip lesions—areas of normal tissue interspersed with inflamed regions. Common symptoms include diarrhea, often without blood, abdominal pain typically localized to the lower right quadrant, weight loss, and malnutrition. Patients may also experience fatigue, fever, and perianal complications such as fissures and abscesses.
2. Ulcerative Colitis (UC)
Ulcerative Colitis is a chronic inflammatory condition that affects only the colon and rectum. The inflammation is continuous, starting in the rectum and extending proximally in a uniform pattern. It is confined to the mucosa and submucosa layers of the bowel wall. Key symptoms include bloody diarrhea, abdominal pain typically in the left lower quadrant, urgency, and tenesmus, which is the sensation of incomplete bowel evacuation. In severe cases, systemic symptoms such as fatigue and weight loss may also be present.
Pathophysiology of Inflammatory Bowel Diseases
1. Genetics: Over 200 genetic loci, including NOD2, IL23R, and ATG16L1, are associated with IBD susceptibility. Genetic predisposition is stronger in Crohn’s disease than ulcerative colitis.
2. Microbiome: Dysbiosis (imbalance of gut microbiota) is commonly observed, with reduced diversity and altered composition. Beneficial bacteria like Faecalibacterium prausnitzii are reduced, while pathogenic bacteria such as Escherichia coli may proliferate.
3. Immune Dysregulation: Overactivation of the immune system leads to persistent inflammation. In CD, a Th1 and Th17-mediated immune response dominates. In UC, a Th2-mediated immune response is more prominent.
4. Environmental Factors:
Smoking: Worsens Crohn’s disease but may have a protective effect in UC.
Diet: High-fat, low-fiber diets can exacerbate inflammation.
Stress: Contributes to symptom flares.
Complications
Crohn’s Disease: Intestinal strictures and obstruction., Fistulas (abnormal connections between organs)., Abscess formation., Nutritional deficiencies (e.g., iron, vitamin B12, vitamin D).
Ulcerative Colitis: Toxic megacolon (severe colonic dilation with risk of perforation)., Increased risk of colorectal cancer., Severe bleeding.
Diagnosis of Inflammatory Bowel Diseases
Diagnosis of IBD involves a combination of clinical evaluation, laboratory tests, imaging, and endoscopy.
1. Laboratory Tests:
Inflammatory Markers: Elevated C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Fecal Calprotectin: Indicates intestinal inflammation.
Anemia and Hypoalbuminemia: Common in severe disease.
2. Imaging:
CT/MR Enterography: Useful for assessing small bowel involvement in Crohn’s disease.
Abdominal Ultrasound: Can detect thickened bowel walls.
3. Endoscopy:
Colonoscopy: Reveals mucosal inflammation, ulcers, or pseudopolyps.
Biopsy confirms histological findings.
4. Serological Tests:
p-ANCA: Often positive in ulcerative colitis.
ASCA (Anti-Saccharomyces cerevisiae antibodies): Common in Crohn’s disease.
Treatment of Inflammatory Bowel Diseases
1. Pharmacological Therapy
Anti-inflammatory Agents: 5-ASA (Mesalamine): First-line for mild to moderate UC. Less effective in Crohn’s disease.
Corticosteroids: Used for acute flares. Not suitable for long-term maintenance due to side effects.
Immunomodulators:
Azathioprine and 6-Mercaptopurine: Effective for maintenance of remission.
Methotrexate: Commonly used in Crohn’s disease.
Biologic Therapy:
Anti-TNF agents (Infliximab, Adalimumab): For moderate to severe IBD.
Integrin inhibitors (Vedolizumab): Target gut-specific inflammation.
IL-12/23 inhibitors (Ustekinumab): Approved for Crohn’s disease.
Small Molecules:
Tofacitinib: Janus kinase (JAK) inhibitor approved for UC.
2. Surgical Management
Crohn’s Disease: Surgery is reserved for complications like strictures, fistulas, or abscesses. Not curative as the disease often recurs.
Ulcerative Colitis: Proctocolectomy with ileal pouch-anal anastomosis (IPAA) can be curative.
Lifestyle and Supportive Measures
- Dietary modifications (e.g., low-residue diet during flares).
- Smoking cessation (especially for Crohn’s disease).
- Stress management techniques (e.g., mindfulness, counseling).
- Regular cancer screenings (e.g., colonoscopy for UC patients).
Future Directions of Inflammatory Bowel Diseases
Microbiome Modulation: Fecal microbiota transplantation (FMT) shows promise in UC.
Precision Medicine: Tailoring treatment based on genetic, microbial, and immune profiling.
Stem Cell Therapy: Mesenchymal stem cells for refractory Crohn’s disease.
IBD is a complex, multifactorial disease requiring a multidisciplinary approach for effective management. Advances in biologic therapies and an improved understanding of the disease’s pathophysiology offer hope for better outcomes. However, challenges remain in achieving long-term remission and preventing complications, necessitating ongoing research and patient education.
Visit to: Pharmacareerinsider.com




