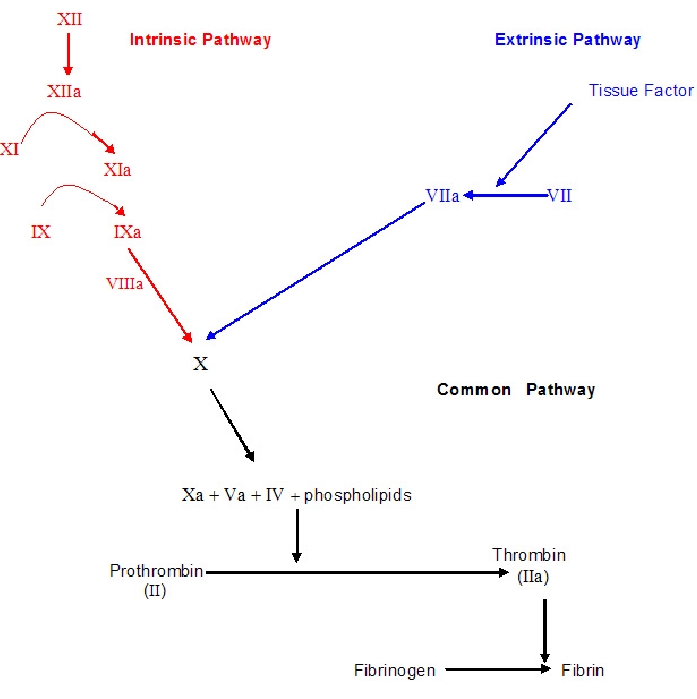
Mechanisms of coagulation: Blood coagulation, or clotting, is a complex and tightly regulated physiological mechanism that prevents excessive bleeding following a vascular injury. It involves a series of sequential and interrelated reactions that ultimately lead to the formation of a blood clot. The coagulation process can be divided into three main pathways: intrinsic, extrinsic, and common.
Mechanisms of coagulation
1. Intrinsic Pathway
The intrinsic pathway, also known as the contact activation pathway, actively initiates within the bloodstream. It typically starts when blood actively comes into contact with foreign surfaces, such as collagen exposed by vessel damage.
The key players in the intrinsic pathway are clotting factors present in the blood, including:
- Factor XII (Hageman factor)
- Factor XI (Pta)
- Factor IX (Christmas factor)
- Factor VIII (Antihemophilic factor)
The intrinsic pathway proceeds as follows
a. Contact with exposed collagen or other activators actively activates Factor XII.
b. Activated factor XII activates factor XI in the presence of prekallikrein and high-molecular-weight kininogen.
c. Activated factor XI then activates factor IX.
d. Factor IX, in the presence of factor VIII, forms a complex that activates factor X.
2. Extrinsic Pathway
The extrinsic pathway actively initiates outside the bloodstream when tissue damage occurs, leading to exposure to tissue factor (TF), also known as factor III.
The extrinsic pathway actively plays a crucial role in rapidly initiating coagulation in response to vascular injury.
The main components of the extrinsic pathway are:
Tissue factor (TF)
Factor VII (Proconvertin)
The extrinsic pathway proceeds as follows:
a. Tissue factor (TF) is released from injured tissues.
b. TF combines with activated factor VII to form the extrinsic tenase complex.
c. The extrinsic tenase complex then activates factor X.
3. Common Pathway
The intrinsic and extrinsic pathways converge to form the common pathway, ultimately forming a stable blood clot.
The common pathway involves several key clotting factors, including:
- Factor X (Stuart-Prower factor)
- Factor V (Labile factor)
- Factor II (Prothrombin)
- Factor I (Fibrinogen)
The common pathway proceeds as follows
a. Factor X combines with factor V to form the prothrombinase complex.
b. The prothrombinase complex converts prothrombin (Factor II) into thrombin (Factor IIa), a critical enzyme in coagulation.
c. Thrombin plays a central role by catalyzing the conversion of soluble fibrinogen into insoluble fibrin strands.
d. Fibrin strands form a mesh that traps blood cells, creating a stable blood clot.
4. Fibrinolysis
Once the blood clot has served its purpose, the body initiates fibrinolysis, a process that dissolves the clot.
- The enzyme plasmin actively breaks down fibrin into soluble fragments.
- Plasmin forms from its precursor, plasminogen, through the action of tissue plasminogen activator (tPA) and other activators.
- Fibrinolysis actively restores normal blood flow once the injury is healed.
The coagulation cascade actively fine-tunes the process, and any disruptions or imbalances can actively lead to bleeding disorders or thrombotic conditions. Various regulatory mechanisms, such as anticoagulants and fibrinolytic factors, actively exist to prevent excessive clot formation and maintain a balance between clotting and bleeding.
Steps involved in coagulation of blood
Blood coagulation, or clotting, involves a sequence of steps to form a stable blood clot when a blood vessel is injured. Here are the key steps in the coagulation of blood:
1. Vasoconstriction (Vascular Phase)
The first response to blood vessel injury is vasoconstriction, where the smooth muscle in the vessel wall contracts to reduce blood flow to the damaged area. This helps minimize blood loss and allows time for subsequent clotting mechanisms to take effect. The process is mediated by vasoconstrictive substances like endothelin, which are released by endothelial cells. The severity of vasoconstriction depends on the extent of the injury.
2. Formation of the Platelet Plug (Primary Hemostasis):
When the inner lining of the blood vessel is disrupted, underlying structures such as collagen and von Willebrand factor (vWF) are exposed. Platelets adhere to these surfaces through specific receptors like glycoprotein Ib. Upon adhesion, platelets become activated, changing their shape and releasing substances like adenosine diphosphate (ADP), thromboxane A2 (TXA2), and serotonin. These mediators recruit additional platelets to the injury site, leading to platelet aggregation. Platelets bind to one another via fibrinogen bridges, reinforced by glycoprotein IIb/IIIa receptors. This process results in the formation of a temporary platelet plug, which provides an initial seal over the injury but requires further stabilization by the coagulation cascade.
3. Coagulation Cascade (Secondary Hemostasis):
The coagulation cascade is a series of enzymatic reactions involving clotting factors that ultimately lead to the formation of a stable fibrin clot. It consists of the intrinsic and extrinsic pathways, both of which converge into a common pathway. The extrinsic pathway is initiated when tissue factor (TF) is released from damaged tissues, activating Factor VII and leading to the activation of Factor X. The intrinsic pathway is triggered when blood comes into contact with negatively charged surfaces, activating Factor XII, followed by a cascade involving Factors XI, IX, and VIII, which also lead to Factor X activation. In the common pathway, activated Factor X (in combination with Factor V) converts prothrombin (Factor II) into thrombin. Thrombin, a key enzyme in coagulation, converts soluble fibrinogen into insoluble fibrin strands. These fibrin strands interlace to form a mesh-like structure that stabilizes the clot. Factor XIII further strengthens the fibrin network by cross-linking the fibrin strands.
4. Clot Retraction
Once the fibrin mesh is formed, the clot undergoes retraction to make it more compact and stable. Platelets within the clot contain contractile proteins like actin and myosin, which pull the fibrin network together, reducing the clot’s size. This process brings the edges of the damaged blood vessel closer together, facilitating the repair process and limiting further bleeding.
5. Fibrinolysis:
After tissue repair is complete, the body must remove the clot to restore normal blood flow. This is achieved through fibrinolysis, a process in which plasminogen (an inactive enzyme incorporated into the clot) is converted into plasmin by tissue plasminogen activator (tPA) and urokinase. Plasmin degrades fibrin into smaller fragments known as fibrin degradation products (FDPs), including D-dimers. This step is essential to prevent excessive clotting and maintain proper circulation.
6. Clot Consolidation and Repair
As the clot is gradually broken down, the body initiates tissue repair by regenerating endothelial cells and connective tissue. Growth factors such as platelet-derived growth factor (PDGF) and vascular endothelial growth factor (VEGF) stimulate the formation of new blood vessels and tissue remodeling. This phase ensures that the blood vessel regains its integrity, allowing normal blood flow to resume without clotting complications.
The coagulation process actively regulates these steps, and any imbalance can lead to bleeding disorders (hemorrhagic) or clotting disorders (thrombotic). The body actively possesses various mechanisms and regulatory factors to balance clotting and bleeding, including anticoagulants and fibrinolytic enzymes. Coagulation actively plays a critical role in preventing excessive blood loss while ensuring normal blood circulation once the injury is healed.

