Oogenesis is the process by which female germ cells, known as oogonia, develop into mature ova (eggs). It is a complex and highly regulated process that occurs within the ovaries, involving several stages of cell division and maturation. Understanding oogenesis is crucial for comprehending female fertility, reproductive health, and the developmental origins of genetic disorders.

Overview of Oogenesis
Oogenesis involves several distinct stages: mitotic division, meiotic division, and cytoplasmic maturation.
1. Mitotic Division (Proliferation Phase)
Oogonia: Oogenesis begins during fetal development when primordial germ cells differentiate into oogonia, which are diploid (2n) stem cells.
Mitosis: Oogonia undergo mitotic divisions to increase their numbers and develop into primary oocytes.
2. Meiotic Division (Maturation Phase)
Primary Oocytes: During fetal development, primary oocytes enter meiosis I but arrest at the diplotene stage of prophase I and remain in this state until puberty.
Puberty: With each menstrual cycle after puberty, a cohort of primary oocytes resumes development.
Meiosis I: Each primary oocyte completes meiosis I, resulting in the formation of two cells: a secondary oocyte and a polar body. Meiosis I is asymmetrical, with the secondary oocyte receiving most of the cytoplasm.
Meiosis II: The secondary oocyte then enters meiosis II but arrests at the metaphase II stage until fertilization occurs. Completion of meiosis II forms a mature ovum (egg) and a second polar body.
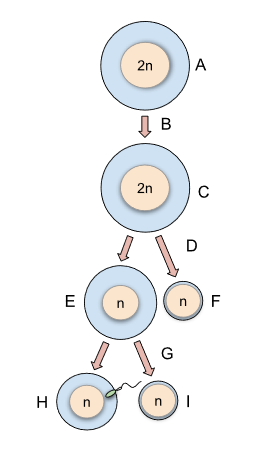
Oogenesis in eukaryotic cells. (A) oogonium where the mitotic division occurs (B) differentiation and meiosis I begins (C) primary oocyte (D) meiosis I is completed and meiosis II begins (E) secondary oocyte (F) first polar body (G) ovulation must occur and the presence of the sperm penetration (fertilization) induces meiosis II to completion (H) ovum (I) second polar body
3. Cytoplasmic Maturation
Oocyte Maturation: During oocyte maturation, the secondary oocyte undergoes changes in cytoplasmic composition and structure, preparing for fertilization.
Cortical Reaction: Following fertilization, the oocyte undergoes the cortical reaction, releasing enzymes to modify the zona pellucida, preventing polyspermy.
Hormonal Regulation of Oogenesis
Oogenesis is regulated by hormonal signals from the hypothalamic-pituitary-gonadal (HPG) axis:
Gonadotropin-Releasing Hormone (GnRH): Secreted by the hypothalamus, GnRH stimulates the release of gonadotropins from the pituitary gland.
Follicle-Stimulating Hormone (FSH): Stimulates follicle growth within the ovaries and promotes the development of primary oocytes.
Luteinizing Hormone (LH): Triggers ovulation and the formation of the corpus luteum, which produces progesterone to support the endometrium.
Ovarian Follicular Development
Oogenesis occurs within ovarian follicles, which are specialized structures within the ovaries:
Primordial Follicles: These are the earliest stage of follicular development, consisting of a primary oocyte surrounded by a single layer of squamous follicular cells.
Primary Follicles: Primordial follicles develop into primary follicles, characterized by the enlargement of the oocyte and the proliferation of follicular cells.
Secondary Follicles: Primary follicles mature into secondary follicles, with the development of an antrum (fluid-filled cavity) surrounding the oocyte.
Graafian Follicle: A mature follicle, also known as a Graafian follicle, is characterized by a large antrum and is ready for ovulation.
Corpus Luteum: After ovulation, the remaining follicular cells form the corpus luteum, which secretes progesterone to support the endometrium.
Factors Influencing Oogenesis
Several factors can influence the process of oogenesis:
Hormonal Imbalances: Disorders affecting the HPG axis, such as polycystic ovary syndrome (PCOS) or ovarian insufficiency, can disrupt oogenesis.
Age: Oogenesis declines with age, with a reduction in the quantity and quality of oocytes.
Environmental Factors: Exposure to toxins, radiation, or certain medications can adversely affect oogenesis.
Genetic Factors: Genetic mutations or chromosomal abnormalities, such as Turner syndrome (XO), can impair oogenesis.
Clinical Relevance and Disorders
Understanding oogenesis is essential for diagnosing and treating female reproductive health conditions:
Ovulatory Disorders: Disorders affecting oogenesis, such as anovulation or premature ovarian failure (POF), can contribute to female infertility.
Assisted Reproductive Technologies (ART): Knowledge of oogenesis informs fertility treatments such as in vitro fertilization (IVF), where mature oocytes are retrieved from ovarian follicles for fertilization in the laboratory.
Ovarian Cancer: Understanding the cellular processes of oogenesis contributes to research into ovarian cancer, a malignancy that can arise from abnormal ovarian cell growth.
Conclusion
Oogenesis is a complex and tightly regulated process that ensures the continuous production of mature ova for female fertility. It involves sequential phases of mitotic and meiotic divisions, followed by cytoplasmic maturation to form mature oocytes capable of fertilization. Hormonal regulation by the HPG axis, cellular interactions within ovarian follicles, and environmental influences all contribute to the process of oogenesis. Understanding the intricacies of oogenesis is crucial for diagnosing and managing female reproductive health conditions and advancing treatments for female infertility. Continued research into oogenesis promises further insights into female fertility and reproductive medicine.
Check this: Pharmacareerinsider.com

