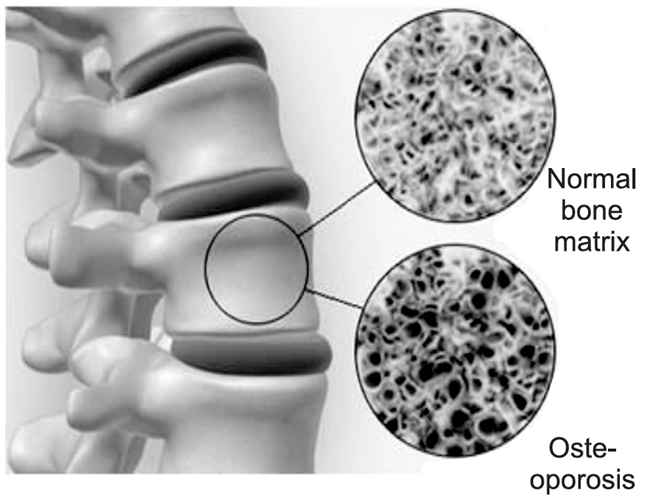
Osteoporosis is a systemic skeletal disorder characterized by reduced bone mass and deterioration of bone tissue, leading to increased bone fragility and susceptibility to fractures. It is often referred to as a “silent disease” because it typically progresses without symptoms until a fracture occurs.
Epidemiology of Osteoporosis
Osteoporosis is a common condition that affects millions of people worldwide, particularly postmenopausal women and elderly individuals. Its prevalence increases with age, with a higher incidence observed in individuals over 50 years old. It is estimated that one in three women and one in five men aged over 50 will experience an osteoporotic fracture in their lifetime. The condition is more common in Caucasians and Asians compared to African Americans. Osteoporosis-related fractures are most commonly seen in the spine, hip, and wrist.
Etiology of Osteoporosis
The development of osteoporosis is influenced by a combination of genetic, environmental, and lifestyle factors. The key factors contributing to osteoporosis include:
1. Genetic Factors: Family history of osteoporosis or fractures. Genetic predisposition affecting bone density and bone turnover.
2. Age: Bone mass decreases with age, particularly after the age of 30, when bone resorption begins to outpace bone formation.
3. Hormonal Changes:
Postmenopausal women: The decrease in estrogen levels following menopause accelerates bone loss.
Men: Decreasing testosterone levels with age can also contribute to osteoporosis, although it tends to occur later than in women.
4. Nutritional Deficiencies:
Calcium: Inadequate calcium intake can result in poor bone mineralization.
Vitamin D: Insufficient vitamin D impairs calcium absorption and bone health.
5. Physical Inactivity: Lack of weight-bearing exercise leads to reduced bone density and increased fracture risk.
6. Medications: Long-term use of glucocorticoids, certain anticonvulsants, and some cancer treatments can lead to osteoporosis.
7. Lifestyle Factors:
Smoking: Smoking impairs bone health by reducing blood flow to the bones and inhibiting bone formation.
Excessive alcohol consumption: Alcohol interferes with the balance of bone remodeling.
8. Other Medical Conditions: Conditions such as rheumatoid arthritis, hyperthyroidism, type 1 diabetes, and eating disorders (e.g., anorexia nervosa) can increase the risk of osteoporosis.
Pathophysiology of Osteoporosis
Osteoporosis occurs due to an imbalance between bone resorption and bone formation. Bone is a dynamic tissue that undergoes constant remodeling throughout life. In healthy individuals, bone resorption (the process by which bone is broken down) is balanced by bone formation (the process by which new bone is made). In osteoporosis:
Increased Bone Resorption: Osteoclast activity (cells that break down bone tissue) increases, leading to excessive loss of bone mass.
Decreased Bone Formation: Osteoblast activity (cells that form new bone) is reduced, impairing the formation of new bone tissue.
As a result, the bone becomes porous and brittle, making it more prone to fractures even with minor trauma or no apparent injury. This weakened bone structure is often characterized by:
- Loss of trabecular (spongy) bone.
- Thinning of cortical bone (the dense outer layer of bone).
- Increased bone fragility, especially in weight-bearing bones such as the spine, hips, and wrists.
Symptoms of Osteoporosis
Osteoporosis often does not cause symptoms until a fracture occurs, making early detection difficult. However, as the disease progresses, the following signs may develop:
Fractures: The most common symptom of osteoporosis is a fracture, which can occur with minimal trauma, such as a fall from standing height or even a sneeze.
Back Pain: Compression fractures in the spine can lead to severe back pain and deformities, such as a loss of height.
Postural Changes: A stooped or hunched posture (kyphosis) may develop due to spinal fractures.
Loss of Height: Individuals may experience gradual height loss due to vertebral fractures.
Tests and Diagnosis of Osteoporosis
The diagnosis of osteoporosis is primarily based on bone mineral density (BMD) testing, along with a review of medical history and risk factors. Key diagnostic tools include:
1. Bone Mineral Density (BMD) Testing:
The Dual-Energy X-ray Absorptiometry (DEXA or DXA) scan is the most common and accurate test used to measure BMD. It compares the density of a person’s bones to the average density of a healthy young adult, expressed as the T-score.
T-score: A score of -1.0 or above is normal; between -1.0 and -2.5 indicates osteopenia (low bone mass), and -2.5 or lower indicates osteoporosis.
Z-score: This compares the BMD to what is expected for someone of the same age, sex, and body size.
2. Fracture Risk Assessment: The FRAX tool is used to estimate the 10-year probability of bone fractures, incorporating factors such as age, sex, smoking, alcohol use, family history, and BMD.
3. Laboratory Tests: Blood tests to assess calcium, vitamin D, and thyroid function may be performed to rule out other conditions contributing to bone loss.
4. Imaging Studies: X-rays may be used to detect fractures or signs of bone loss, though they are not typically used for diagnosing osteoporosis itself.
Treatments and Drugs of Osteoporosis
The primary goals of osteoporosis treatment are to prevent fractures, maintain bone mass, and reduce bone pain. Treatment includes pharmacological therapy and lifestyle modifications:
1. Lifestyle Changes:
Diet: Adequate intake of calcium and vitamin D is essential for bone health. The recommended daily intake for adults is around 1,000 mg of calcium and 800-1,000 IU of vitamin D.
Exercise: Weight-bearing exercises, such as walking, jogging, and strength training, help maintain bone density and improve balance to reduce the risk of falls.
Fall Prevention: Home safety measures, such as removing tripping hazards and using assistive devices, may reduce fracture risk.
2. Pharmacological Treatments:
Bisphosphonates: These are the most commonly prescribed drugs for osteoporosis. They work by inhibiting osteoclast-mediated bone resorption, thus increasing bone mass.
Examples: Alendronate (Fosamax), Risedronate (Actonel), Ibandronate (Boniva).
Selective Estrogen Receptor Modulators (SERMs): SERMs mimic estrogen’s protective effects on bones and help prevent bone loss.
Example: Raloxifene (Evista).
Calcitonin: A hormone that helps regulate calcium levels and bone metabolism. It is typically used in postmenopausal women who cannot tolerate other treatments.
Example: Nasal spray (Miacalcin).
Denosumab: A monoclonal antibody that inhibits osteoclast formation, reducing bone resorption.
Example: Prolia.
Parathyroid Hormone (PTH) Analogs: These stimulate new bone formation and are used in severe cases of osteoporosis.
Examples: Teriparatide (Forteo), Abaloparatide (Tymlos).
Hormone Replacement Therapy (HRT): Estrogen therapy may be considered for postmenopausal women, although it is generally avoided due to potential risks of cardiovascular disease and breast cancer.
Strontium Ranelate:
A medication that can increase bone formation and decrease bone resorption, although its use is limited due to safety concerns.
3. Pain Management: Analgesics, such as acetaminophen, NSAIDs, or prescription pain relievers, may be used to manage pain from fractures or back pain.
Osteoporosis is a progressive disease that significantly increases the risk of fractures, particularly in older adults. Early detection through BMD testing and appropriate treatment can help manage the disease and reduce fracture risk. Medications like bisphosphonates, SERMs, and PTH analogs, along with lifestyle changes, play a crucial role in maintaining bone health and preventing complications associated with osteoporosis.
Visit to: Pharmacareerinsider.com