Parasympathomimetics, also known as cholinergic agonists or muscarinic agonists, are drugs that mimic the action of the parasympathetic nervous system by stimulating the cholinergic receptors. These receptors are predominantly found in various organs and tissues throughout the body, including the heart, smooth muscles, exocrine glands, and central nervous system.
Classification of Parasympathomimetics
Parasympathomimetics can be classified into two main groups based on their mechanism of action:
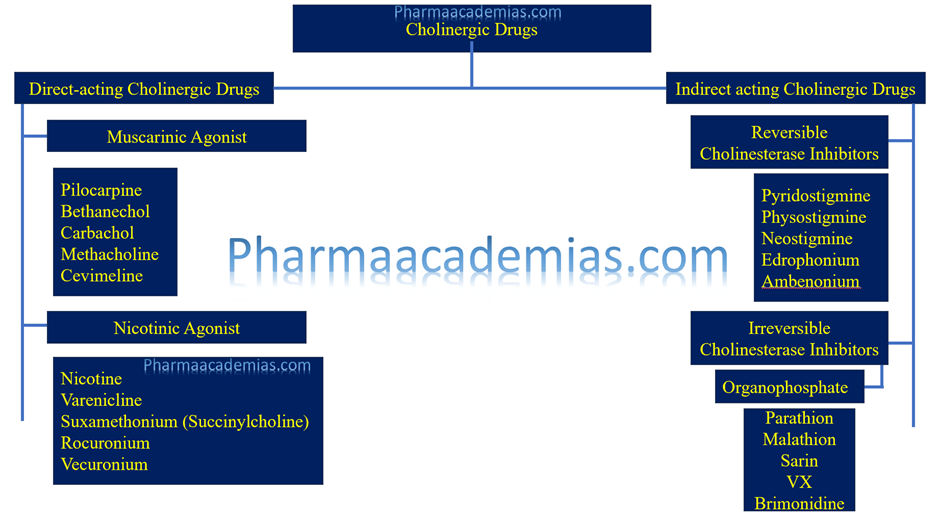
1. Direct-acting parasympathomimetics:
These drugs directly bind to and activate cholinergic receptors, mimicking the action of acetylcholine. Examples include:
– Bethanechol: Bethanechol is a direct-acting parasympathomimetic drug that primarily stimulates muscarinic receptors, leading to smooth muscle contraction, particularly in the gastrointestinal and urinary tracts. It is a synthetic choline ester and acts as a structural analog of acetylcholine.
– Pilocarpine: Pilocarpine is a direct-acting parasympathomimetic alkaloid derived from the South American shrub Pilocarpus jaborandi. It acts primarily as a muscarinic receptor agonist, mimicking the effects of acetylcholine, and is commonly used in ophthalmology for the treatment of glaucoma and xerostomia (dry mouth).
– Carbachol: Carbachol is a synthetic choline ester that acts as a direct-acting parasympathomimetic agent, primarily stimulating muscarinic receptors with some activity on nicotinic receptors. It is structurally similar to acetylcholine but more resistant to degradation by cholinesterases, resulting in prolonged pharmacological effects.
2. Indirect-acting parasympathomimetics
These drugs increase the concentration of acetylcholine at the receptor sites by inhibiting acetylcholinesterase, the enzyme responsible for acetylcholine degradation. Examples include:
Physostigmine: Physostigmine acts similarly to neostigmine as an indirect-acting cholinergic agonist by inhibiting acetylcholinesterase. It increases acetylcholine levels in the central and peripheral nervous systems. Physostigmine is used to reverse the effects of anticholinergic toxicity, such as those caused by certain medications or plants, by increasing cholinergic activity and restoring normal physiological function.
Neostigmine: Neostigmine is an indirect-acting cholinergic agonist that inhibits the activity of acetylcholinesterase, the enzyme responsible for breaking down acetylcholine. This inhibition leads to increased acetylcholine levels at cholinergic synapses and prolonged stimulation of cholinergic receptors. It is used to treat myasthenia gravis, a neuromuscular disorder characterized by muscle weakness, by increasing muscle strength through enhanced cholinergic neurotransmission at the neuromuscular junction.
Donepezil: Donepezil drugs are also indirect-acting cholinergic agonists that inhibit acetylcholinesterase, leading to increased acetylcholine levels in the brain. They primarily affect central cholinergic neurotransmission.
Donepezil is used in the treatment of Alzheimer’s disease to improve cognitive function and alleviate symptoms associated with cholinergic deficits in the brain.
Pharmacological Actions of Parasympathomimetics
Parasympathomimetics exert their effects by activating cholinergic receptors, primarily muscarinic receptors (M receptors) and nicotinic receptors (N receptors). The pharmacological actions include:
1. Cardiovascular Effects:
Bradycardia: Direct activation of cardiac muscarinic receptors leads to decreased heart rate.
Vasodilation: Stimulation of muscarinic receptors on vascular endothelium leads to vasodilation, primarily in skin and mucous membranes.
2. Respiratory Effects:
Bronchoconstriction: Stimulation of muscarinic receptors in bronchial smooth muscles leads to bronchoconstriction.
Increased secretions: Activation of muscarinic receptors in bronchial glands increases mucus secretion.
3. Gastrointestinal Effects:
Increased gastrointestinal motility: Activation of muscarinic receptors in the gastrointestinal tract enhances peristalsis.
Increased secretion: Stimulation of muscarinic receptors in the gastrointestinal glands increases secretion of saliva, gastric acid, and other digestive enzymes.
4. Genitourinary Effects:
Contraction of detrusor muscle: Activation of muscarinic receptors in the bladder wall leads to increased bladder contraction, promoting urination.
5. Ophthalmic Effects:
Constriction of pupils (miosis): Activation of muscarinic receptors on the iris sphincter muscle leads to pupil constriction.
Increased aqueous humor outflow: Stimulation of muscarinic receptors in the ciliary body promotes aqueous humor drainage, reducing intraocular pressure.
Indications of Parasympathomimetics
Parasympathomimetics are used in the treatment of various medical conditions, including:
1. Urinary Retention: Bethanechol is used to stimulate bladder contraction in patients with urinary retention or neurogenic bladder dysfunction.
2. Glaucoma: Pilocarpine is used to reduce intraocular pressure by promoting the drainage of aqueous humor in the treatment of glaucoma.
3. Xerostomia: Pilocarpine is also used to stimulate salivary gland secretion in patients with dry mouth (xerostomia) due to radiation therapy or Sjögren’s syndrome.
4. Myasthenia Gravis: Neostigmine and pyridostigmine are used as adjunctive therapy in the management of myasthenia gravis, a neuromuscular disorder characterized by muscle weakness and fatigue.
5. Alzheimer’s Disease: Donepezil is used in the treatment of Alzheimer’s disease to improve cognitive function by inhibiting the breakdown of acetylcholine in the brain.
Contraindications of Parasympathomimetics
Parasympathomimetics are contraindicated in certain conditions due to their potential to exacerbate symptoms or cause adverse effects. Contraindications include:
1. Bradycardia or Heart Block: Parasympathomimetics can worsen bradycardia or heart block and are contraindicated in patients with these conditions.
2. Asthma or Chronic Obstructive Pulmonary Disease (COPD): Parasympathomimetics can exacerbate bronchoconstriction and are contraindicated in patients with asthma or COPD.
3. Peptic Ulcer Disease: Parasympathomimetics can increase gastric acid secretion and worsen peptic ulcer disease. They are contraindicated in patients with active ulcers.
4. Urinary Obstruction: Parasympathomimetics can exacerbate urinary obstruction and are contraindicated in patients with bladder outlet obstruction.
5. Angle-Closure Glaucoma: Parasympathomimetics can precipitate an acute angle-closure glaucoma attack and are contraindicated in patients with this condition.
6. Hypersensitivity: Patients with a known hypersensitivity to parasympathomimetic drugs or their components should not use these medications.
Parasympathomimetics plays a crucial role in the management of various medical conditions by mimicking the actions of the parasympathetic nervous system. Understanding their classification, pharmacological actions, dosage, indications, and contraindications is essential for their safe and effective use in clinical practice. Healthcare professionals should carefully evaluate patients’ medical history and individual characteristics before prescribing parasympathomimetic medications to optimize therapeutic outcomes and minimize potential risks.

