Menstruation, also known as the menstrual cycle or menses, is a complex physiological process that occurs in females of reproductive age. It involves the cyclical shedding of the endometrium (the lining of the uterus) and is regulated by intricate interactions between hormones from the hypothalamus, pituitary gland, ovaries, and uterus. Understanding the physiology of menstruation is essential for comprehending reproductive health, fertility, and various menstrual-related disorders.
Phases of the Menstrual Cycle
The menstrual cycle is typically divided into several phases, each characterized by distinct hormonal changes and physiological events:
1. Menstrual Phase
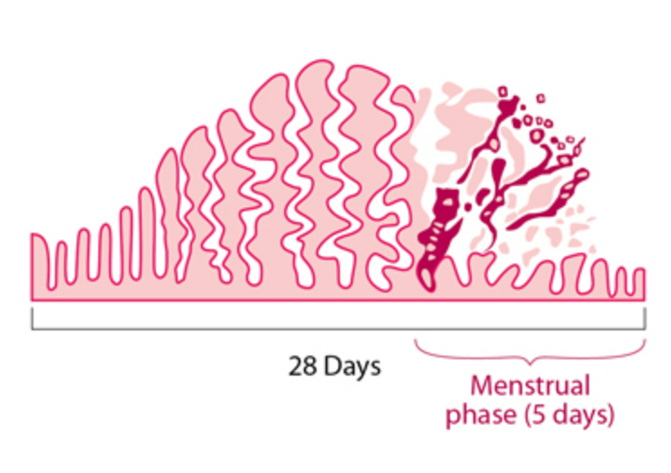
Duration: Approximately 3-7 days.
Hormonal Events: At the beginning of menstruation, levels of estrogen and progesterone drop sharply due to the regression of the corpus luteum (if pregnancy did not occur).
Physiological Events: The shedding of the endometrial lining occurs, resulting in menstrual bleeding. This bleeding consists of blood, mucus, and tissue from the inner lining of the uterus.
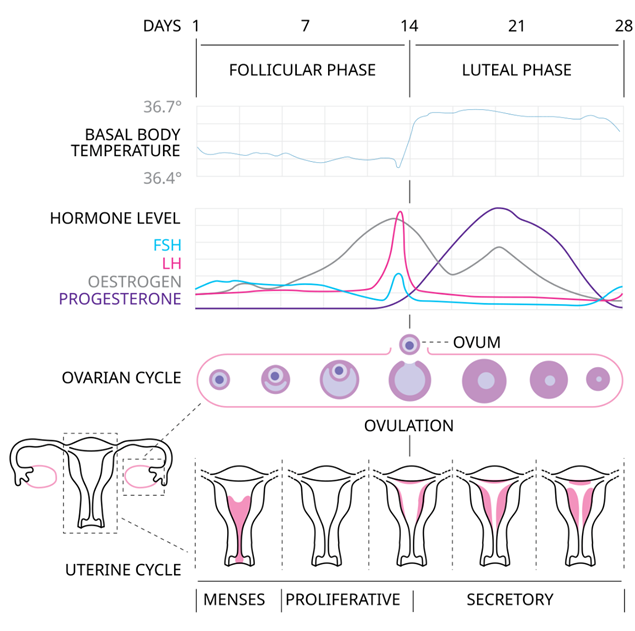
2. Proliferative Phase (Follicular Phase)
Duration: Approximately days 6-14 of the menstrual cycle.
Hormonal Events: As menstruation ends, the pituitary gland releases follicle-stimulating hormone (FSH), which stimulates the growth of ovarian follicles. The developing follicles produce increasing amounts of estrogen.
Physiological Events: Estrogen stimulates the thickening and proliferation of the endometrial lining in preparation for potential implantation of a fertilized egg. This phase culminates in ovulation.
3. Ovulatory Phase
Duration: Typically occurs around day 14 of a 28-day cycle.
Hormonal Events: A surge in luteinizing hormone (LH), triggered by rising estrogen levels, induces ovulation— the release of a mature egg (ovum) from one of the ovaries.
Physiological Events: The mature ovum is released from the ovarian follicle and is swept into the fallopian tube, where it may be fertilized by sperm. The remainder of the follicle transforms into the corpus luteum.
4. Luteal Phase
Duration: Approximately days 15-28 of the menstrual cycle.
Hormonal Events: The corpus luteum secretes progesterone and estrogen, preparing the endometrium for potential implantation of a fertilized egg.
Physiological Events: If fertilization does not occur, hormone levels decline towards the end of the luteal phase. This drop in hormones causes vasoconstriction in the endometrial blood vessels, leading to ischemia and subsequent shedding of the endometrial lining, initiating the next menstrual phase.
Hormonal Regulation of Menstruation
Hypothalamic-Pituitary-Ovarian Axis
Gonadotropin-Releasing Hormone (GnRH): Secreted by the hypothalamus, GnRH stimulates the anterior pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
Follicle-Stimulating Hormone (FSH): Stimulates the growth and maturation of ovarian follicles, which produce estrogen.
Estrogen: Produced primarily by developing ovarian follicles, estrogen stimulates the proliferation of the endometrial lining during the proliferative phase.
Luteinizing Hormone (LH): Triggers ovulation and promotes the formation of the corpus luteum.
Progesterone: Produced by the corpus luteum, progesterone maintains the endometrial lining during the luteal phase and prepares it for potential implantation.
Endometrial Changes
The endometrium undergoes dynamic changes throughout the menstrual cycle under the influence of estrogen and progesterone:
Proliferative Phase: Estrogen stimulates the proliferation of endometrial glands and blood vessels, thickening the endometrial lining.
Secretory Phase (During Luteal Phase): Progesterone from the corpus luteum induces glandular secretion and maintains the endometrium in preparation for embryo implantation.
Menstrual Phase: Decreasing levels of estrogen and progesterone cause vasoconstriction of endometrial blood vessels, leading to tissue ischemia and shedding of the endometrial layer.
Menstrual Disorders
Dysmenorrhea
Primary Dysmenorrhea: Painful menstrual cramps without underlying pathology, often due to increased prostaglandin production.
Secondary Dysmenorrhea: Painful periods caused by pelvic pathology, such as endometriosis or fibroids.
Menorrhagia
Excessive menstrual bleeding, often due to hormonal imbalances, uterine fibroids, or bleeding disorders.
Amenorrhea
Primary Amenorrhea: Absence of menstruation by age 16 with no secondary sexual characteristics or by age 14 with no menstruation.
Secondary Amenorrhea: Cessation of menstruation for at least 3 cycles or 6 months in women who previously had regular cycles.
Factors Influencing the Menstrual Cycle
Various factors can influence the menstrual cycle:
Nutritional Status: Severe calorie restriction or eating disorders (e.g., anorexia nervosa) can disrupt hormonal balance and lead to amenorrhea.
Stress: Physical or emotional stress can affect the hypothalamic-pituitary-ovarian axis, causing irregularities in menstrual cycles.
Medications: Certain medications, such as hormonal contraceptives or treatments for other medical conditions, can alter menstrual patterns.
Environmental Factors: Exposure to environmental toxins, pollutants, or extreme changes in climate can impact menstrual regularity.
The physiology of menstruation involves a complex interplay of hormones, neuroendocrine signals, and tissue changes within the female reproductive system. Each phase of the menstrual cycle is finely orchestrated to prepare the uterus for potential pregnancy or to initiate the shedding of the endometrial lining if fertilization does not occur. Understanding the nuances of menstrual physiology is crucial for diagnosing and managing menstrual disorders, optimizing fertility, and promoting overall reproductive health in women. Continued research into menstrual physiology and its regulation contributes to advancements in women’s health care and reproductive medicine
Visit to: Pharmacareerinsider.com

