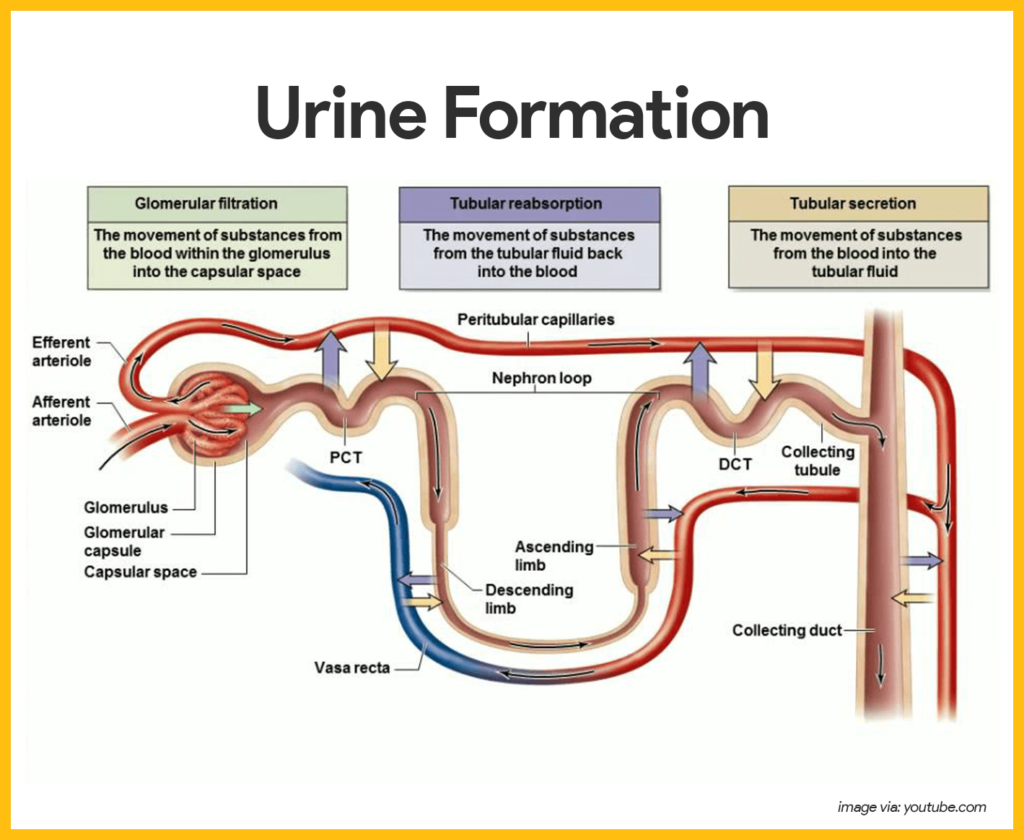
The process of urine formation, also known as renal physiology, involves intricate mechanisms that regulate the composition and volume of urine produced by the kidneys. It consists of three main processes: glomerular filtration, tubular reabsorption, and tubular secretion. Let’s explore each in detail:
1. Glomerular Filtration
Glomerular filtration occurs in the renal corpuscles within the nephrons, the functional units of the kidneys. The key structures involved in this process include:
Glomerulus: A network of capillaries formed by the afferent arteriole, which brings blood into the glomerulus, and the efferent arteriole, which carries blood away. The glomerulus acts as a filtration barrier.
Bowman’s Capsule: A double-walled, cup-shaped structure that surrounds the glomerulus and collects the filtrate.
Filtration Membrane: Consists of three layers: fenestrated endothelium of the glomerular capillaries, basement membrane, and podocytes (specialized cells of the Bowman’s capsule). This membrane allows small molecules such as water, ions, glucose, and waste products to pass through while retaining larger proteins and blood cells.
During glomerular filtration Blood pressure forces plasma through the filtration membrane into Bowman’s capsule, forming the glomerular filtrate. Filtration is primarily driven by the hydrostatic pressure of the blood in the glomerular capillaries (glomerular filtration pressure).
2. Tubular Reabsorption
Tubular reabsorption occurs in the renal tubules and involves the selective reabsorption of essential substances from the glomerular filtrate back into the bloodstream. Key features include:
Proximal Convoluted Tubule (PCT): The majority of reabsorption occurs here. It reabsorbs about 65-70% of filtered water, sodium, glucose, amino acids, and other solutes.
Loop of Henle: Reabsorption of water and ions occurs here, particularly in the descending limb (water) and ascending limb (ions).
Distal Convoluted Tubule (DCT) and Collecting Duct: Fine-tuning of reabsorption occurs, regulated by hormones such as aldosterone, antidiuretic hormone (ADH), and atrial natriuretic peptide (ANP).
3. Tubular Secretion
Tubular secretion involves the active transport of substances from the bloodstream into the renal tubules. It helps eliminate waste products, regulate pH, and control electrolyte balance. Key points include:
– Secretion primarily occurs in the proximal and distal convoluted tubules and the collecting ducts.
– Substances secreted include hydrogen ions, potassium ions, drugs, and metabolic waste products such as creatinine and ammonia.
Regulation of Urine Formation
Several factors regulate urine formation to maintain homeostasis:
Renal Blood Flow and Glomerular Filtration Rate (GFR): Regulated by mechanisms such as autoregulation, neural control, and hormonal control (e.g., renin-angiotensin-aldosterone system).
Hormonal Regulation: Hormones such as aldosterone, ADH, and ANP regulate water and electrolyte balance by influencing reabsorption and secretion processes.
Autonomic Nervous System: Sympathetic and parasympathetic nervous systems modulate renal blood flow and GFR.
Intrinsic Regulation: Intrinsic mechanisms within the kidneys, such as tubuloglomerular feedback, help maintain a stable GFR.
Clinical Considerations:
Disorders affecting urine formation, such as kidney disease, hypertension, diabetes mellitus, and electrolyte imbalances, can lead to abnormal urine volume, composition, and renal function. Understanding the physiology of urine formation is crucial for diagnosing and managing these conditions effectively.
In summary, urine formation is a complex process involving glomerular filtration, tubular reabsorption, and tubular secretion, regulated by various physiological mechanisms. This intricate process ensures the excretion of waste products while maintaining the body’s fluid and electrolyte balance.

