The reticuloendothelial system (RES), also known as the mononuclear phagocyte system (MPS), is a highly specialized and intricate network of cells and tissues distributed throughout the body. It plays a critical role in immune defense, blood filtration, tissue homeostasis, and metabolic regulation. This system is primarily responsible for phagocytosis, in which specialized cells engulf and digest foreign particles, microorganisms, aged or damaged cells, and cellular debris. Additionally, it serves as a key component in immune surveillance and antigen presentation, making it an essential part of both innate and adaptive immunity.
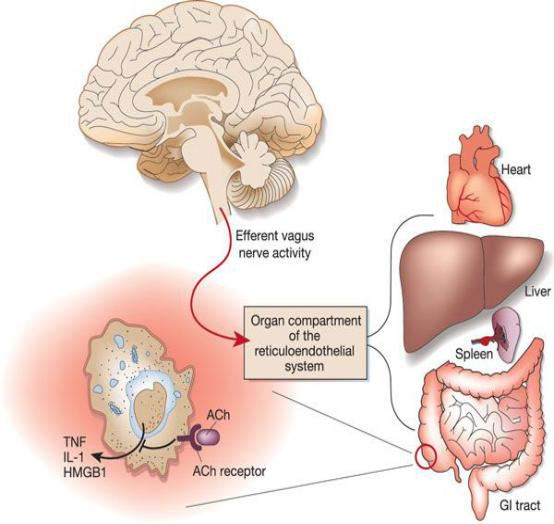
The RES consists of monocytes, macrophages, dendritic cells, and reticular cells, which are distributed across different tissues and organs such as the bone marrow, liver, spleen, lymph nodes, and the vascular endothelium. These cells work in concert to maintain immune balance and protect the body against infections, autoimmune diseases, and other pathological conditions.
Here are some essential aspects of the reticuloendothelial system:
1. Monocytes
Monocytes are a type of white blood cell (leukocyte) that plays a crucial role in the immune response. They are produced in the bone marrow and circulate in the bloodstream before migrating into tissues, where they differentiate into macrophages or dendritic cells.
Functions of Monocytes:
- Phagocytosis: Monocytes engulf and digest bacteria, viruses, fungi, and cellular debris, contributing to the body’s first line of defense.
- Antigen Presentation: They process and present pathogen-derived antigens to T lymphocytes, activating the adaptive immune response.
- Inflammatory Regulation: Monocytes release cytokines and chemokines, which modulate inflammation and recruit other immune cells to infection sites.
- Tissue Repair: By secreting growth factors, monocytes help in wound healing and tissue regeneration.
2. Macrophages
Macrophages are vital immune cells that defend against infections, remove debris, and engage in the innate immune system. They excel at phagocytosis, engulfing and digesting pathogens, dead cells, and more. Distributed throughout the body, they continuously monitor for infections or damage, efficiently eliminating microorganisms like bacteria and viruses. Macrophages play a pivotal role in initiating immune responses by presenting antigens to cells like T cells and initiating specific immune reactions. They are essential for maintaining tissue health, aiding wound healing, and ensuring proper immune system function.
3. Dendritic Cells
In the adaptive immune response, dendritic cells have a critical role, especially in initiating immune reactions against pathogens. These immune cells specialize in presenting antigens by capturing, processing, and presenting them from invading microorganisms like bacteria or viruses to other immune cells, notably T cells. Dendritic cells’ presentation of antigens serves as a crucial trigger for specific immune responses against encountered pathogens. They are considered key players in bridging the innate and adaptive immune systems and are vital for the body’s ability to recognize and respond to a wide range of infectious agents.
4. Reticular Cells
Reticular cells are stromal cells found in various lymphoid organs and tissues. They create a supportive network for immune cells and contribute to the structural integrity of these organs.
Functions of Reticular Cells:
- Structural Support: They provide a scaffolding for immune cell migration and organization within lymphoid tissues.
- Cytokine Secretion: Reticular cells produce chemokines that guide lymphocytes to their designated sites.
- Extracellular Matrix Formation: They maintain the fibrous architecture of lymphoid tissues.
5. Functions
The reticuloendothelial system has several crucial functions, including:
- Phagocytosis: The system’s cells engulf and digest bacteria, viruses, dead cells, and foreign particles.
- Antigen Presentation: Dendritic cells and macrophages present antigens to other immune cells, triggering immune responses.
- Immune Surveillance: The system continuously monitors the body for invading pathogens and abnormalities.
- Hematopoiesis: Certain reticuloendothelial cells participate in the production of blood cells in the bone marrow.
6. Organs and Tissues
1. Liver (Kupffer Cells): Kupffer cells are liver-resident macrophages that clear toxins, dead cells, and microbes from blood entering via the portal vein.
2. Spleen: The spleen acts as a blood filter, removing senescent RBCs and producing immune responses against bloodborne pathogens.
3. Bone Marrow: Contains hematopoietic stem cells (HSCs) and reticular cells that regulate blood cell formation.
4. Lymph Nodes: Macrophages and dendritic cells in lymph nodes capture antigens from lymphatic fluid and present them to T and B lymphocytes.
5. Lungs (Alveolar Macrophages): Alveolar macrophages clear inhaled pathogens and pollutants, ensuring proper lung function.
Disorders of the Reticuloendothelial System
Dysfunctions in the RES can lead to a variety of immune-related disorders:
1. Immunodeficiency Disorders: Primary immunodeficiencies (e.g., chronic granulomatous disease, Chediak-Higashi syndrome) impair phagocytic function. Acquired immunodeficiency (e.g., HIV/AIDS) affects macrophage and dendritic cell function.
2. Autoimmune Diseases: Overactive immune responses can contribute to conditions like rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE).
3. Hemophagocytic Lymphohistiocytosis (HLH): A rare but severe hyperinflammatory disorder characterized by excessive macrophage activation and uncontrolled cytokine release.
4. Chronic Inflammatory Diseases: Dysfunctional macrophages contribute to conditions like atherosclerosis, inflammatory bowel disease (IBD), and pulmonary fibrosis.

