Severe Acute Respiratory Syndrome (SARS) is a viral respiratory illness caused by the SARS coronavirus (SARS-CoV). The outbreak of SARS in 2002-2003 marked a significant global public health crisis. SARS is characterized by severe respiratory symptoms and can lead to acute respiratory distress syndrome (ARDS) and, in some cases, death.
Etiopathogenesis:
1. Viral Transmission:
SARS-CoV is primarily transmitted through respiratory droplets when an infected person coughs, sneezes, or talks.
Close person-to-person contact is a common mode of transmission.
2. Zoonotic Origin:
The virus is believed to have originated in bats and transmitted to humans through intermediate hosts, possibly civets in the case of the 2002-2003 outbreak.
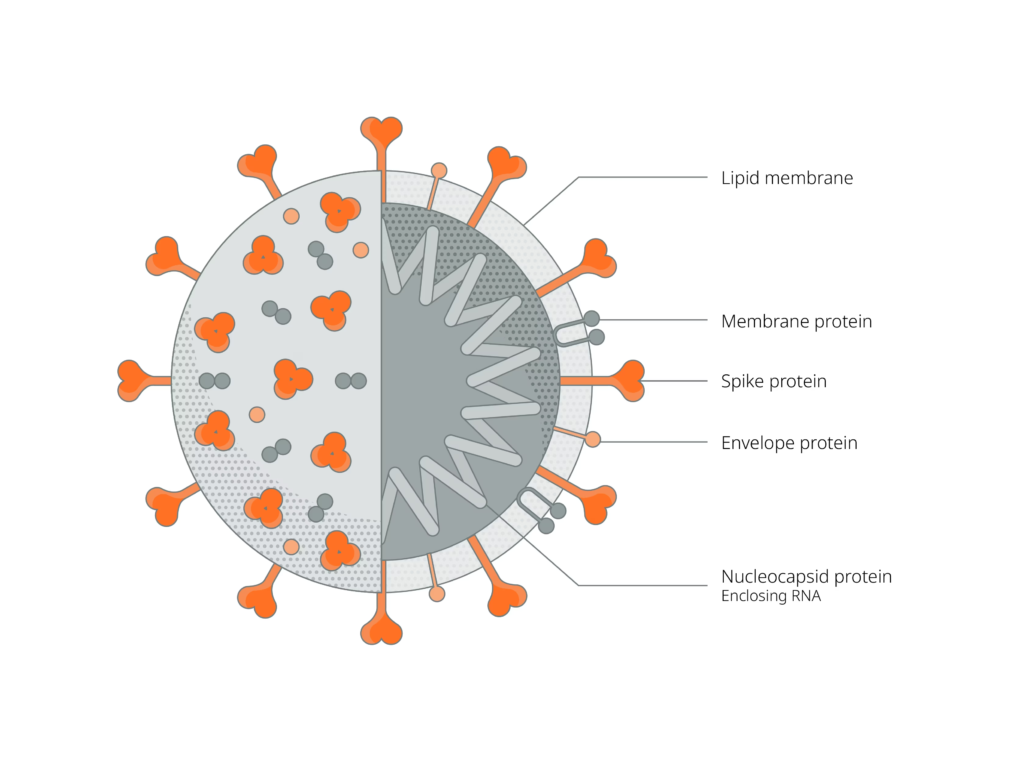
3. Viral Entry and Replication:
The virus enters human cells by binding to angiotensin-converting enzyme 2 (ACE2) receptors, which are prevalent in the respiratory tract.
Viral replication occurs in the respiratory epithelial cells, leading to the release of viral particles and further infection.
Clinical Manifestations:
1. Incubation Period:
– Typically 2 to 10 days from exposure to symptom onset.
2. Respiratory Symptoms:
– Fever, cough, and shortness of breath are common.
– Progression to pneumonia and respiratory failure, particularly in severe cases.
3. Non-Respiratory Symptoms:
– Headache, myalgia, and gastrointestinal symptoms such as diarrhea.
4. Complications:
– Acute respiratory distress syndrome (ARDS) characterized by severe respiratory failure.
– Multiorgan failure and shock in severe cases.
Nonpharmacological Management:
1. Isolation and Infection Control:
– Strict isolation measures to prevent the spread of the virus.
– Personal protective equipment for healthcare workers and caregivers.
2. Supportive Care:
– Oxygen therapy and mechanical ventilation for respiratory support.
– Intravenous fluids to maintain hydration.
3. Quarantine Measures:
– Implementation of quarantine protocols to control the spread of the virus in affected areas.
Pharmacological Management:
1. Antiviral Medications: Ribavirin, lopinavir/ritonavir, and other antivirals were used in the early management of SARS, although their efficacy remains a subject of debate.
2. Corticosteroids: Used in some cases to mitigate the inflammatory response and reduce lung injury. However, their use is controversial due to potential side effects.
3. Antibiotics: Administered to manage secondary bacterial infections.
4. Investigational Therapies: During the SARS outbreak, various experimental treatments were explored, including convalescent plasma therapy.
Follow-up and Prognosis:
Regular Monitoring: Regular monitoring of clinical status, oxygen levels, and radiological findings.
Complications and Long-Term Effects: Surveillance for potential complications such as post-acute sequelae of SARS (PASC), also known as “long COVID.”
Prognosis: The overall mortality rate for SARS was around 10%, with higher rates in older adults and those with underlying health conditions.
Public Health Measures: Implementation of public health measures, including contact tracing, to control the spread of the virus and prevent further outbreaks.
In conclusion, SARS represents a severe respiratory illness caused by the SARS-CoV. The management involves a combination of nonpharmacological measures, supportive care, and, in some cases, experimental pharmacological interventions. Strict infection control measures and ongoing research efforts are critical in responding to emerging viral threats like SARS.

