A thalassemia is a group of inherited blood disorders characterized by the body’s inability to produce sufficient and functional hemoglobin, resulting in anemia. Hemoglobin, the protein in red blood cells responsible for carrying oxygen, has two main components: alpha and beta globin chains. Thalassemia is categorized based on which globin chain is affected: alpha thalassemia or beta thalassemia. This note explores the causes, pathophysiology, symptoms, diagnosis, treatment, and prevention of thalassemia.
Causes of Thalassemia
Thalassemia is caused by mutations in the genes responsible for the production of hemoglobin chains:
1. Alpha Thalassemia: Results from deletions or mutations in the HBA1 and HBA2 genes on chromosome 16, affecting alpha globin production. Severity depends on the number of affected genes (one to four).
2. Beta Thalassemia: Caused by mutations in the HBB gene on chromosome 11, affecting beta globin production. Severity depends on the specific mutations and whether one or both beta globin genes are affected.
Pathophysiology of Thalassemia
Thalassemia affects hemoglobin production, leading to an imbalance in the globin chains. This imbalance results in ineffective erythropoiesis (production of red blood cells) and chronic hemolysis (destruction of red blood cells):
1. Alpha Thalassemia: Insufficient alpha chains cause excess beta or gamma chains, forming unstable hemoglobin tetramers. Severity ranges from silent carriers (one gene affected) to hemoglobin H disease (three genes affected) and hydrops fetalis (four genes affected).
2. Beta Thalassemia: Reduced or absent beta chains cause excess alpha chains, which precipitate and damage red blood cells. Classified into three main types: beta thalassemia minor (one gene affected), beta thalassemia intermedia (milder form with moderate anemia), and beta thalassemia major (Cooley’s anemia, severe anemia).
Symptoms of Thalassemia
The symptoms of thalassemia vary based on the type and severity of the disease:
1. Alpha Thalassemia:
– Silent Carrier: No symptoms.
– Alpha Thalassemia Trait: Mild anemia, often asymptomatic.
– Hemoglobin H Disease: Moderate to severe anemia, jaundice, splenomegaly (enlarged spleen), and skeletal abnormalities.
– Hydrops Fetalis: Severe anemia in utero, often fatal without intrauterine intervention.
2. Beta Thalassemia:
– Beta Thalassemia Minor: Mild anemia, often asymptomatic.
– Beta Thalassemia Intermedia: Moderate anemia, splenomegaly, bone deformities, and growth retardation.
– Beta Thalassemia Major: Severe anemia, requiring regular blood transfusions, growth retardation, skeletal abnormalities, jaundice, and organ damage due to iron overload from transfusions.
Diagnosis of Thalassemia
Diagnosis of thalassemia involves a combination of medical history, physical examination, and laboratory tests:
1. Medical History and Physical Examination: Assessing family history of thalassemia or anemia, growth patterns, and physical signs like jaundice and splenomegaly.
2. Laboratory Tests:
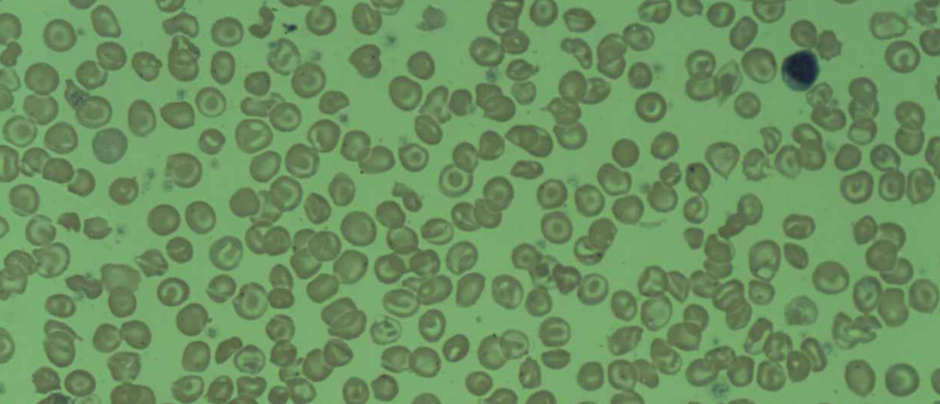
Complete Blood Count (CBC): Microcytic hypochromic anemia, low mean corpuscular volume (MCV), and mean corpuscular hemoglobin (MCH).
Hemoglobin Electrophoresis: Identifies abnormal hemoglobin variants and quantifies hemoglobin A, A2, and F.
Genetic Testing: Detects specific gene mutations responsible for alpha or beta thalassemia.
Peripheral Blood Smear: Shows microcytosis, hypochromia, target cells, and nucleated red blood cells.
Treatment of Thalassemia
The treatment of thalassemia aims to manage symptoms, prevent complications, and improve quality of life:
1. Blood Transfusions: Regular transfusions for severe cases (e.g., beta thalassemia major) to maintain adequate hemoglobin levels and prevent complications.
2. Iron Chelation Therapy: Used to remove excess iron from the body due to frequent blood transfusions, preventing iron overload and related organ damage (e.g., deferoxamine, deferasirox).
3. Folic Acid Supplementation: Supports red blood cell production and reduces anemia.
4. Splenectomy: Surgical removal of the spleen in cases of severe splenomegaly or increased red blood cell destruction.
5. Bone Marrow/Stem Cell Transplant: Potential cure for thalassemia, particularly in severe cases, though limited by donor availability and associated risks.
6. Gene Therapy: Emerging treatment approach aiming to correct the genetic defect responsible for thalassemia.
Prevention of Thalassemia
Preventive measures for thalassemia include:
1. Genetic Counseling: For individuals with a family history of thalassemia to understand their risk and reproductive options.
2. Prenatal Screening: Genetic testing during pregnancy to determine if the fetus has thalassemia or is a carrier.
3. Carrier Screening: Testing potential parents, especially in populations with a high prevalence of thalassemia, to identify carriers and assess the risk of having affected children.
Conclusion
Thalassemia is a complex genetic disorder with significant health implications. Understanding the genetic basis, pathophysiology, symptoms, diagnosis, treatment, and prevention of thalassemia is crucial for effective management and improving patient outcomes. Advances in medical care, genetic counseling, and emerging therapies continue to enhance the quality of life for individuals with thalassemia, emphasizing the importance of early diagnosis, comprehensive care, and ongoing support.

