Anatomy of the Heart: The human heart is the organ that pumps blood throughout the body via the vessels of the circulatory system, supplying oxygen and nutrients to the tissues and removing carbon dioxide and other wastes. Pumping blood through the arteries, capillaries, and veins is the major function of the heart. It maintains a proper circulation of blood. The human heart functions throughout a person’s lifespan and is responsible for the survival of living beings. The heart is almost the size of a large fist and weighs between about 280 to 340 grams in men and 230 to 280 grams in women.
Anatomy of the Heart
Chambers of the Heart
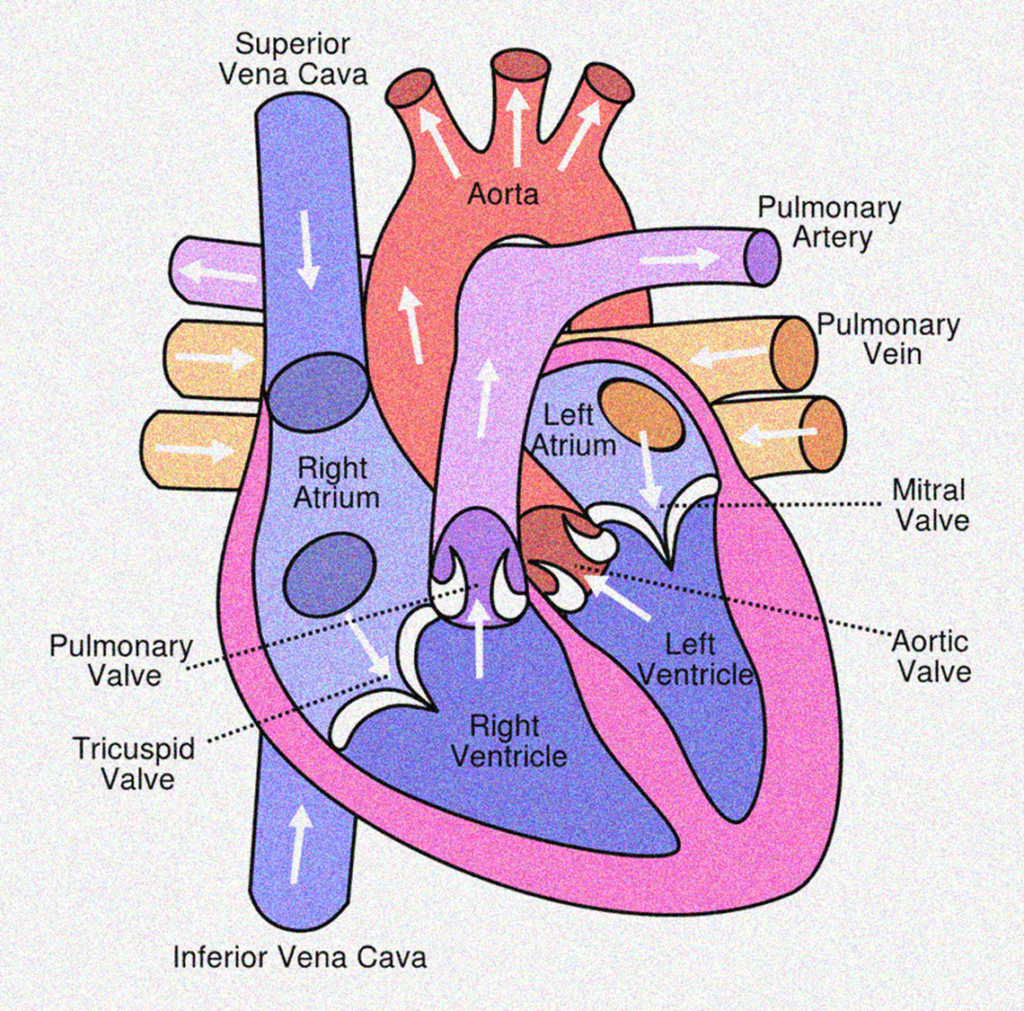
Our heart has 4 chambers, The heart’s upper chambers are the right and left atria, with relatively thin walls separated by a common myocardial wall called the interatrial septum. The lower chambers are the right and left ventricles with thicker walls and the interventricular septum separates them. As you can see, the atria receive blood from either the body or the lungs and the ventricles pump blood into the lungs or the body.
1. Right Atrium: The two big veins return blood to the right atrium from the body. The upper vena cava carries upper-body blood, and the lower vena cava carries lower-body blood. Blood flows into the right ventricle from the right atrium through the right atrioventricular (AV) valve or the tricuspid valve. The tricuspid valve consists of three endocardium flaps (or cusps) strengthened by connective tissue. All valves in the circulatory system have the general purpose of preventing blood backflow. The purpose of the tricuspid valve is to prevent the flow of blood from the right ventricle to the right atrium when contracting the right ventricle. As the ventricle contracts, blood is forced to close the valve behind three-valve flaps.
2. Right Ventricle: The tricuspid valve closes when the right ventricle contracts and the blood is pumped through the pulmonary artery (or trunk) to the lungs. The pulmonary semilunar valve is at the junction of this large artery and the right ventricle. When the right ventricle contracts and pumps blood into the pulmonary artery, its three flaps are forced open. Blood tends to come back when the right ventricle relaxes, but this fills the valve flaps and closes the pulmonary valve to prevent blood from flowing back into the right ventricle.
3. Left Atrium: In the left atrium, blood comes from the lungs through four pulmonary veins. This blood flows through the left atrioventricular (AV) valve into the left ventricle, also known as the mitral valve or bicuspid valve. When the left ventricle contracts, the mitral valve prevents blood from the left ventricle to the left atrium.
Another function of the atria is to produce a hormone that is involved in maintaining blood pressure. When increased blood volume or blood pressure stretches the atria’s walls, the cells produce atrial natriuretic peptide (ANP), also known as the atrial natriuretic hormone (ANH).
ANP decreases kidney reabsorption of sodium ions to excrete more sodium ions in urine, which in turn increases water removal. Water loss reduces the volume of blood and blood pressure. You might have noticed that ANP is an antagonist to the aldosterone hormone, which increases blood pressure.
4. Left Ventricle: The left ventricle walls are thicker than the right ventricle walls, allowing the left ventricle to contract more vigorously. The left ventricle, through the aorta, the body’s largest artery, pumps blood to the body. At the junction between the aorta and the left ventricle is the aortic semilunar valve. The left ventricle’s contraction force, which also closes the mitral valve, opens this valve.
When the left ventricle relaxes, the aortic valve closes to prevent blood from the aorta to the left ventricle. When the mitral valve closes, it prevents the backflow of blood to the left atrium; the flaps of the mitral valve are also anchored by chordae tendineae and papillary muscles.
The right side of the heart receives deoxygenated blood from the body and pumps it into the lungs for oxygen collection and carbon dioxide release. The heart’s left side receives oxygenated blood from the lungs, pumping it into the body. Both pumps work simultaneously, i.e. both atria and ventricles contract together.
Valves of the Heart
The human heart contains four main valves that regulate blood flow and ensure that it moves in the correct direction through the heart’s chambers and into the circulatory system. These valves prevent the backflow of blood and play a critical role in maintaining efficient circulation.
1. Tricuspid Valve: The tricuspid valve is one of the atrioventricular (AV) valves located between the right atrium and the right ventricle. It is composed of three cusps or flaps and plays a vital role in regulating blood flow from the right atrium into the right ventricle. During ventricular contraction (systole), the tricuspid valve closes to prevent the backflow of blood into the atrium, ensuring that it moves forward into the pulmonary circulation via the pulmonary artery.
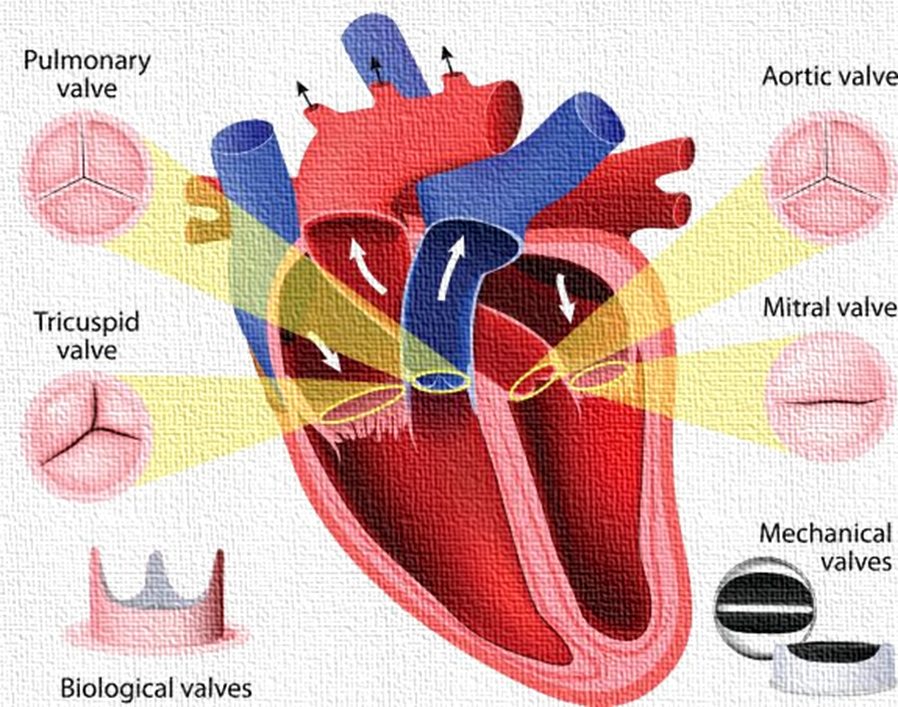
2. Mitral Valve: Also known as the bicuspid valve, the mitral valve is the other atrioventricular valve, situated between the left atrium and the left ventricle. It has two cusps and ensures one-way blood flow from the left atrium into the left ventricle. When the left ventricle contracts, the mitral valve closes tightly to prevent the regurgitation of blood back into the atrium, allowing efficient pumping of oxygen-rich blood into the systemic circulation through the aorta.
3. Pulmonary Valve: The pulmonary valve is a semilunar valve located at the junction of the right ventricle and the pulmonary artery. It consists of three semilunar cusps that open when the right ventricle contracts, allowing deoxygenated blood to flow into the pulmonary artery and onward to the lungs for oxygenation. When the ventricle relaxes, the valve closes to prevent blood from flowing back into the right ventricle.
4. Aortic Valve: Positioned between the left ventricle and the aorta, the aortic valve is another semilunar valve with three cusps. It opens when the left ventricle contracts, permitting oxygenated blood to enter the aorta and be distributed throughout the body. Upon relaxation of the ventricle, the aortic valve closes to stop any reverse flow of blood into the left ventricle, maintaining the directional flow needed for effective systemic circulation.
Septa of the Heart
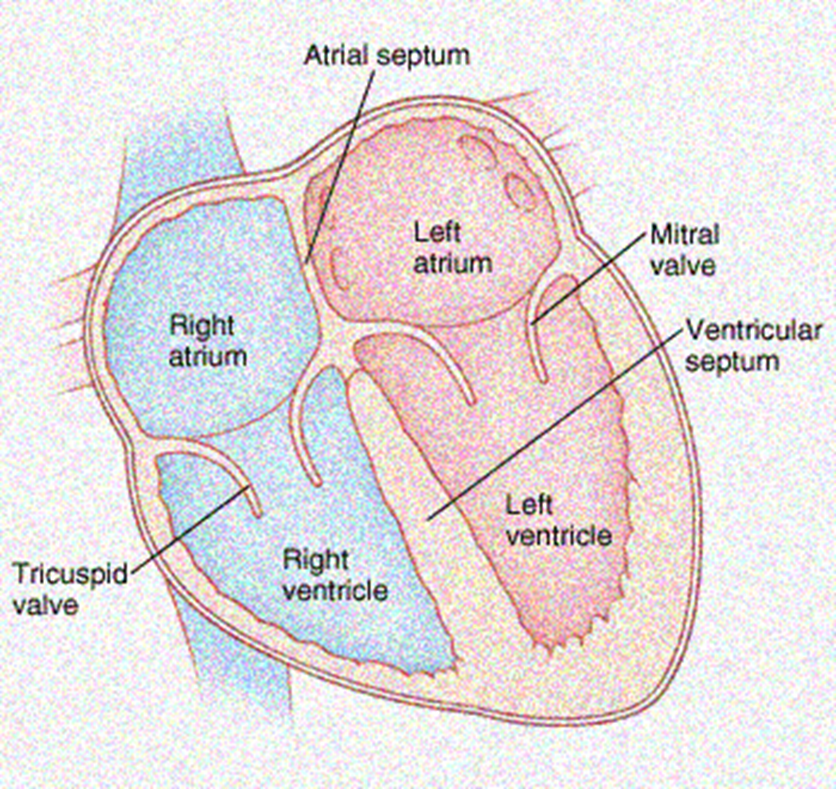
Septa (singular: septum) in the heart are muscular or membranous walls that separate different heart chambers. These septa play a critical role in maintaining the one-way flow of blood through the heart and ensuring the efficient functioning of the cardiovascular system. Here’s a note on the main septa found in the heart:
1. Interatrial Septum: The interatrial septum is a wall that separates the two upper chambers of the heart, the right atrium and the left atrium. Its primary function is to prevent the mixing of oxygenated and deoxygenated blood. Oxygen-rich blood from the lungs enters the left atrium, while deoxygenated blood from the body enters the right atrium.
2. Interventricular Septum: The interventricular septum is a sturdy wall separating the heart’s two lower chambers, the right ventricle and the left ventricle.

This septum ensures oxygen-poor blood in the right ventricle is pumped into the pulmonary circulation. In contrast, oxygen-rich blood in the left ventricle is pumped into the systemic circulation.
Common Heart Conditions and Disorders
- Arrhythmia – Abnormal heart rhythms (too fast, too slow, or irregular).
- Cardiomyopathy – Thickening, stiffening, or enlargement of the heart muscle.
- Congestive Heart Failure – The heart is too weak or stiff to pump blood effectively.
- Coronary Artery Disease – Plaque buildup leading to narrowed coronary arteries.
- Myocardial Infarction (Heart Attack) – Blockage in a coronary artery causing loss of oxygen to part of the heart muscle.
- Heart Valve Disease – Malfunction of one or more heart valves.
- Pericarditis – Inflammation of the pericardial sac surrounding the heart.
- Hypertension – High blood pressure exerting excessive force on artery walls.
- Hypercholesterolemia – Elevated cholesterol levels increasing the risk of blockages.
- Diabetes – Elevated blood glucose levels that can damage cardiovascular tissues over time.
Common Symptoms of Heart Conditions
- Chest pain or discomfort
- Heart palpitations
- Dizziness or lightheadedness
- Shortness of breath
- Fatigue or general weakness
- Swelling in the legs, ankles, or abdomen
Common Diagnostic Tests
- Blood pressure measurement
- Electrocardiogram (ECG or EKG)
- Echocardiogram
- Chest X-ray
- Blood tests (e.g., lipid profile, cardiac enzymes)
- Cardiac catheterization
- Computed Tomography (CT) scan
- Magnetic Resonance Imaging (MRI)
- Exercise or pharmacologic stress test
Common Treatments for Heart Conditions
- Medications (e.g., antihypertensives, anticoagulants, antiarrhythmics)
- Lifestyle changes (e.g., diet, exercise, smoking cessation)
- Medical devices (e.g., pacemakers, implantable defibrillators)
- Minimally invasive procedures (e.g., angioplasty, catheter ablation)
- Surgical interventions (e.g., coronary artery bypass grafting, valve repair/replacement)
Heart Care and Maintenance
How to Keep Your Heart Healthy?
If you have a diagnosed heart condition, it’s essential to follow your healthcare provider’s treatment plan. This includes taking prescribed medications on time and in the correct dosage.
In addition to medical management, the following lifestyle changes can significantly support heart health:
- Maintain a healthy body weight.
- Consume alcohol only in moderation, if at all.
- Follow a heart-healthy diet rich in fruits, vegetables, whole grains, and lean proteins.
- Engage in regular physical activity—at least 150 minutes of moderate exercise per week.
- Limit sodium (salt) intake to help control blood pressure.
- Manage stress through healthy techniques such as meditation, deep breathing, or journaling.
- Quit smoking and avoid the use of tobacco products. Also, stay away from secondhand smoke. If you are a smoker, consult your healthcare provider for support and resources to help you quit.
Questions to Ask Your Healthcare Provider
Being informed about your heart health is essential. You may consider asking the following questions during your next appointment:
- How does my family history influence my risk of heart disease?
- What steps can I take to lower my blood pressure?
- How do my cholesterol levels affect my heart health?
- What are the warning signs of a heart attack?
- What dietary changes should I make to reduce the risk of heart disease?
Final Note
Your heart is the central organ of the circulatory system. It pumps blood and supplies oxygen and nutrients to all parts of the body. Given its vital role, protecting your heart should be a lifelong priority.
While heart diseases are common, many are preventable or manageable through lifestyle changes and medical care. Regular check-ups, a healthy lifestyle, and early detection can significantly enhance your heart health and overall quality of life.


1 thought on “The Heart: Anatomy and Functions”