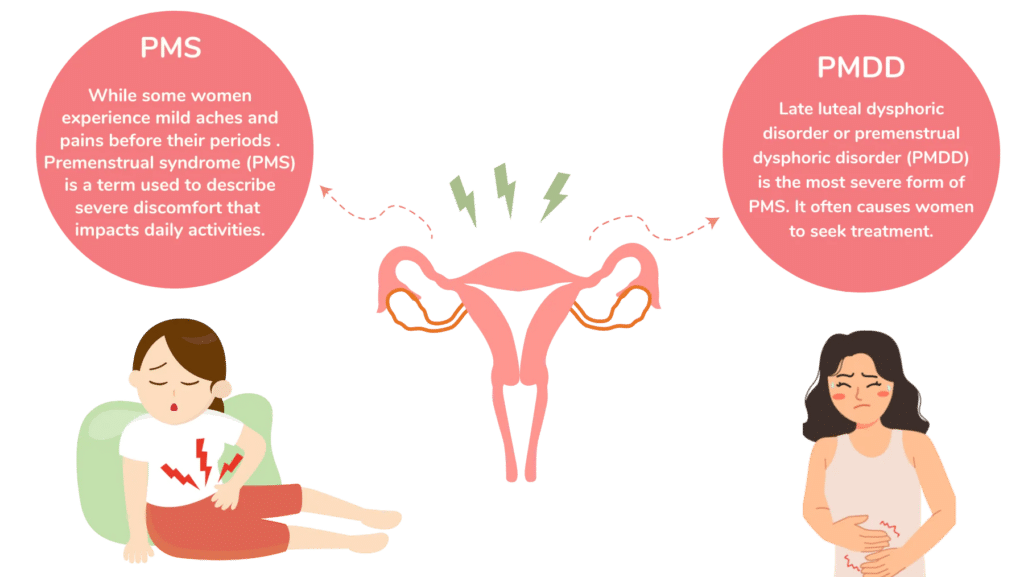
Premenstrual dysphoric disorder (PMDD) is a severe and often debilitating form of premenstrual syndrome (PMS), affecting around 3-8% of individuals with menstrual cycles. Unlike PMS, which causes mild physical and emotional symptoms before menstruation, PMDD brings intense mood swings, anxiety, irritability, and depressive episodes that can severely impact daily functioning and relationships. In this blog, we will explore what PMDD is, its symptoms, causes, risk factors, diagnosis, and available treatment options.
What is Premenstrual Dysphoric Disorder?
PMDD is classified as a mood disorder associated with the menstrual cycle, typically occurring a week or two before menstruation and resolving shortly after the period begins. PMDD is more intense and often disrupts work, school, social activities, and interpersonal relationships.
Key Characteristics of PMDD:
- Symptoms appear during the luteal phase (the period between ovulation and the start of menstruation) and subside shortly after menstruation begins.
- Symptoms recur in most cycles, distinguishing PMDD from other mood disorders.
- Unlike PMS, PMDD symptoms are primarily psychological and are intense enough to interfere significantly with daily life.
Symptoms of PMDD
PMDD symptoms can be grouped into emotional, physical, and behavioral categories. To be diagnosed with PMDD, an individual must experience at least five of these symptoms, with at least one of the first four.
1. Emotional Symptoms
- Mood Swings: Extreme mood changes, often described as emotional rollercoasters, marked by intense sadness, crying spells, and feelings of hopelessness.
- Irritability and Anger: Heightened irritability or anger, often directed at oneself or others, leading to strained relationships.
- Anxiety and Tension: Feelings of being on edge, anxious, or highly stressed, often without a clear trigger.
- Depression and Low Self-Esteem: A sense of worthlessness, despair, and low self-worth that can sometimes lead to suicidal thoughts.
2. Physical Symptoms
- Fatigue and Low Energy: Persistent fatigue and difficulty in performing daily tasks, even with adequate rest.
- Changes in Sleep: Insomnia or oversleeping, both of which exacerbate mood disturbances.
- Physical Pain: Headaches, joint pain, muscle aches, and abdominal bloating are common.
- Breast Tenderness and Swelling: Many individuals report breast tenderness and an increase in breast size before menstruation.
3. Behavioral Symptoms
Difficulty Concentrating: Lack of focus or mental clarity, affecting performance at work or school.
Appetite Changes: Increased cravings or binge eating, especially for carbohydrates or sweets.
Social Withdrawal: A tendency to avoid social interactions and activities due to irritability or low mood.
Uncontrolled Emotions: Crying spells or emotional outbursts that feel unmanageable and often occur without a clear reason.
Causes of PMDD
The exact cause of PMDD remains unknown, but it is believed to stem from an abnormal response to hormonal fluctuations that occur during the menstrual cycle. Research suggests that individuals with PMDD may be genetically predisposed to an exaggerated response to these hormone changes.
Key Contributing Factors:
Hormonal Sensitivity: Unlike PMS, PMDD is not simply due to fluctuating hormone levels but rather to a heightened sensitivity to these changes. This sensitivity primarily involves the hormones estrogen and progesterone.
Neurotransmitter Changes: PMDD may involve imbalances in brain chemicals such as serotonin, which affects mood regulation. Hormonal fluctuations can impact serotonin levels, contributing to symptoms like mood swings, depression, and anxiety.
Genetic Predisposition: Studies suggest that individuals with a family history of PMDD or other mood disorders may be at a higher risk.
Lifestyle and Environmental Factors: High stress levels, lack of exercise, poor sleep, and a diet lacking essential nutrients can exacerbate PMDD symptoms.
Risk Factors for PMDD
While PMDD can affect anyone with a menstrual cycle, certain factors may increase susceptibility.
Family History: A family history of mood disorders, depression, or anxiety may raise the risk.
Mental Health Disorders: Individuals with a history of depression, anxiety, or bipolar disorder are more likely to experience PMDD.
Environmental Stressors: Traumatic life events, chronic stress, or a lack of social support can contribute to PMDD symptoms.
Age: PMDD symptoms are most common in women in their late 20s to early 40s, particularly those who experience irregular menstrual cycles.
Diagnosing PMDD
PMDD is typically diagnosed by a healthcare provider based on the individual’s medical history, symptom patterns, and exclusion of other mood disorders. The process often involves tracking symptoms over two menstrual cycles to confirm the timing and severity.
Diagnostic Criteria (DSM-5):
- According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), PMDD diagnosis requires:
- Five or more symptoms during most menstrual cycles over the past year.
- Symptoms severe enough to interfere with work, social activities, or relationships.
- Symptoms are not an exacerbation of another disorder, such as major depression or generalized anxiety.
Treatment Options for PMDD
Effective treatment for PMDD often involves a combination of lifestyle modifications, medication, and therapy. Here are some of the most common treatment options.
1. Lifestyle Modifications
Exercise: Regular physical activity has been shown to boost mood and reduce stress, helping to manage PMDD symptoms.
Dietary Changes: A balanced diet rich in complex carbohydrates, whole grains, fruits, vegetables, and lean proteins can help stabilize mood and energy levels.
Stress Reduction: Yoga, meditation, and deep-breathing exercises can help manage stress, reducing the intensity of symptoms.
Adequate Sleep: Prioritizing quality sleep can help improve emotional resilience and reduce irritability.
2. Medications
Antidepressants: Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine and sertraline, are often prescribed to manage PMDD symptoms. They can be taken continuously or only during the luteal phase, depending on individual needs.
Hormonal Treatments: Birth control pills, especially those with a low estrogen dose, can help regulate hormone levels and reduce symptoms. GnRH agonists, which suppress the menstrual cycle, are sometimes used for severe cases.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Pain relievers like ibuprofen or naproxen can alleviate physical symptoms like breast tenderness, headaches, and muscle aches.
Diuretics: These can help reduce bloating and water retention, a common symptom of PMDD.
3. Cognitive Behavioral Therapy (CBT)
CBT is a type of talk therapy that can help individuals manage their response to PMDD symptoms by recognizing and changing negative thought patterns. CBT can be particularly beneficial for reducing irritability, mood swings, and anxiety.
4. Nutritional Supplements
Calcium: Studies suggest that calcium supplements can help reduce PMDD symptoms, particularly mood swings, fatigue, and food cravings.
Magnesium: Magnesium supplementation may ease water retention, breast tenderness, and mood disturbances.
Vitamin B6: This vitamin is believed to help regulate mood-related symptoms, although its effectiveness can vary between individuals.
5. Alternative Therapies
Some individuals find relief with alternative approaches, although these should be used in consultation with a healthcare provider:
Acupuncture: This traditional practice may help alleviate physical pain and improve overall well-being.
Herbal Remedies: Chasteberry (Vitex agnus-castus) and St. John’s Wort have been explored as natural remedies, though they may interact with other medications, so it’s essential to consult a healthcare provider before use.
Coping Strategies for PMDD
Living with PMDD can be challenging, but certain strategies can help individuals better manage symptoms:
Symptom Tracking: Keeping a journal to track emotional and physical symptoms can provide insight into patterns, making it easier to predict and prepare for symptom onset.
Support Networks: Joining support groups or connecting with others who experience PMDD can offer emotional relief and practical advice.
Routine Self-Care: Engaging in regular self-care activities, such as spending time in nature, practicing mindfulness, and setting boundaries, can help improve overall mental well-being.
When to Seek Help
If PMDD symptoms interfere with daily functioning, or if thoughts of self-harm or hopelessness arise, it’s crucial to seek medical advice. Effective treatments are available, and a healthcare provider can tailor a treatment plan based on individual needs.
Final Thoughts
Premenstrual dysphoric disorder is a complex condition, but with the right treatment approach, individuals can effectively manage symptoms and lead fulfilling lives. By recognizing the symptoms, understanding the causes, and exploring treatment options, those affected by PMDD can take proactive steps toward improved mental and physical well-being.

