Urinary Tract Infections
Urinary Tract Infections (UTIs) are one of the most common bacterial infections encountered globally, affecting individuals across all age groups, with a pronounced prevalence among women. A UTI can involve any part of the urinary system, which includes the kidneys, ureters, bladder, and urethra. While generally curable with timely antibiotic therapy, untreated or recurrent UTIs can lead to serious complications such as pyelonephritis, chronic kidney disease, and sepsis.
UTIs not only impose a significant clinical burden but also represent a substantial economic cost to healthcare systems. Understanding the microbial causes, risk factors, clinical manifestations, and management strategies is vital for proper diagnosis and prevention.
2. Definition
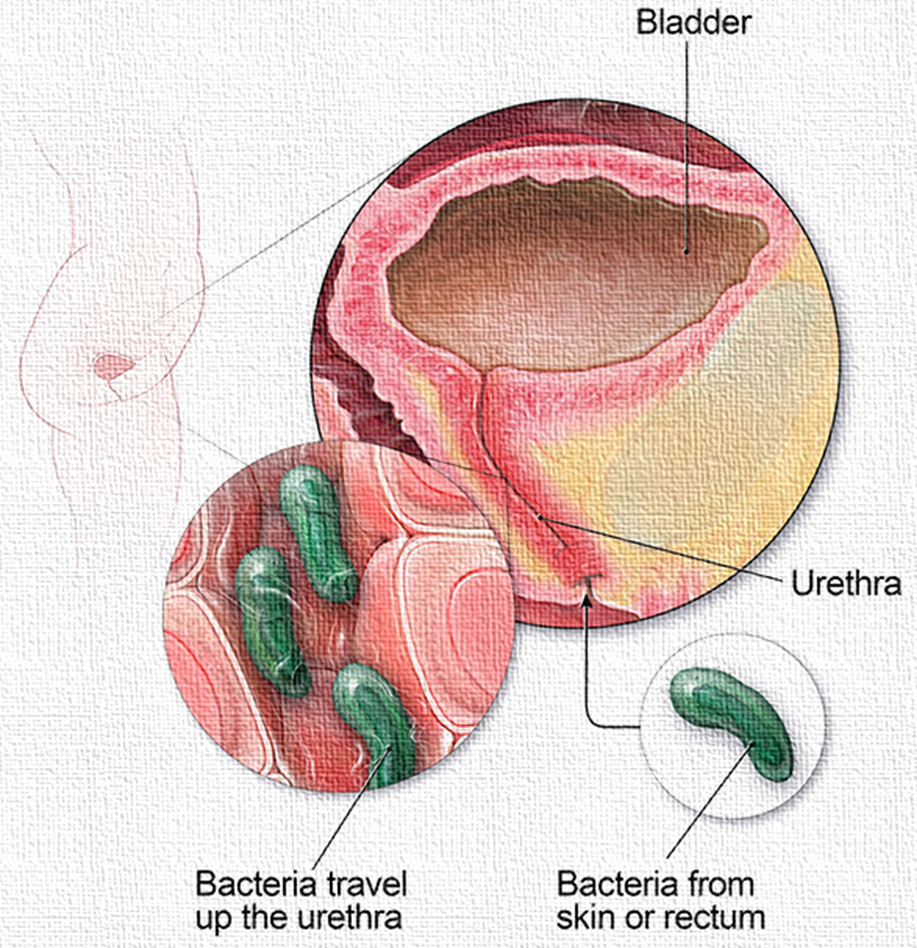
A urinary tract infection (UTI) is defined as an infection caused by the invasion and multiplication of pathogenic microorganisms—primarily bacteria—in the urinary tract, leading to inflammation and clinical symptoms. Depending on the location, UTIs are categorized as lower UTIs (cystitis and urethritis) or upper UTIs (pyelonephritis).
3. Epidemiology of Urinary Tract Infections
3.1 Prevalence
- UTIs are second only to respiratory infections as the most common type of infection.
- Annually, about 150 million people worldwide are diagnosed with UTIs.
- Women are disproportionately affected—nearly 50–60% of women will experience a UTI at least once in their lifetime.
- Recurrent UTIs affect 20–30% of women after an initial infection.
3.2 Age and Gender Distribution
- In infants, boys have a higher risk due to congenital anomalies.
- In adult women, UTIs are more common due to anatomical and hormonal factors.
- Postmenopausal women are also at increased risk due to estrogen deficiency.
- Elderly men are prone to UTIs primarily because of prostatic enlargement and urinary stasis.
3.3 Healthcare-Associated UTIs (HAUTIs)
- Common in hospitalized patients, especially those with indwelling catheters.
- Account for up to 40% of nosocomial infections.
4. Etiology and Pathogenesis
4.1 Causative Microorganisms
Bacteria are the predominant cause of UTIs. The most common pathogens include:
- Escherichia coli (E. coli) – accounts for 75–95% of uncomplicated UTIs.
- Klebsiella pneumoniae
- Proteus mirabilis
- Enterococcus faecalis
- Pseudomonas aeruginosa – especially in complicated and nosocomial UTIs.
- Staphylococcus saprophyticus – typically affects young, sexually active females.
4.2 Virulence Mechanisms
- Adhesion to uroepithelial cells via pili or fimbriae.
- Biofilm formation in chronic or catheter-associated infections.
- Urease production by Proteus spp., leading to struvite stone formation.
- Evasion of immune responses, such as intracellular persistence and inhibition of phagocytosis.
5. Causes and Risk Factors
5.1 Anatomical and Physiological Factors
- Short urethra in females
- Prostatic hypertrophy in elderly men
- Pregnancy-induced urinary stasis
5.2 Behavioral and Environmental Factors
- Poor perineal hygiene
- Sexual activity (honeymoon cystitis)
- Use of diaphragms or spermicides
5.3 Medical and Iatrogenic Factors
- Diabetes mellitus
- Immunosuppression
- Urinary catheters and invasive urological procedures
- Nephrolithiasis (kidney stones)
6. Types of UTIs
6.1 Based on Site of Infection
A. Lower UTIs
- Cystitis: Infection of the bladder
- Symptoms: dysuria, urgency, frequency, suprapubic pain, hematuria
- Urethritis: Infection of the urethra
- Symptoms: burning sensation during urination, discharge (in some STIs)
B. Upper UTIs
- Pyelonephritis: Infection of the kidney parenchyma
- Symptoms: flank pain, high fever, chills, nausea, vomiting, costovertebral angle tenderness
6.2 Based on Complication Status
Uncomplicated UTI
- Occurs in otherwise healthy, non-pregnant women
- No structural or functional abnormalities
Complicated UTI
- Occurs in patients with comorbidities, pregnancy, anatomical abnormalities, or indwelling devices
- Higher risk of treatment failure and recurrence
6.3 Based on Recurrence
Relapse
- Recurrence of infection by the same organism within 2 weeks of treatment
Reinfection
- Infection by a different organism or the same organism after 2 weeks
7. Clinical Manifestations
7.1 Lower UTIs (Cystitis)
- Dysuria (painful urination)
- Increased urinary frequency and urgency
- Suprapubic pain or discomfort
- Cloudy, foul-smelling urine
- Hematuria (in some cases)
7.2 Upper UTIs (Pyelonephritis)
- High-grade fever with chills
- Flank or back pain
- Nausea and vomiting
- Malaise and fatigue
- Costovertebral angle tenderness
7.3 UTIs in Special Populations
- Elderly patients may present with confusion or falls without urinary symptoms.
- Children may show irritability, poor feeding, or fever without source.
- Pregnant women may develop asymptomatic bacteriuria, which needs treatment to avoid complications.
8. Diagnosis of Urinary Tract Infections
8.1 Urinalysis
- Dipstick tests: leukocyte esterase (WBCs) and nitrites (produced by bacteria)
- Microscopic analysis: presence of pyuria, bacteriuria, RBCs, epithelial cells
8.2 Urine Culture
- Gold standard for diagnosis
- Significant bacteriuria: ≥10⁵ CFU/mL in clean-catch midstream sample
- Identifies organism and antibiotic sensitivity
8.3 Imaging Studies
- Ultrasound or CT scan: used in recurrent, complicated, or upper UTIs
- Intravenous pyelogram (IVP): for structural evaluation
9. Treatment of Urinary Tract Infections
9.1 Uncomplicated UTI (Empirical Therapy)
- Nitrofurantoin (5–7 days)
- Trimethoprim-sulfamethoxazole (3–5 days) – if local resistance is <20%
- Fosfomycin (single dose)
- Pivmecillinam (in some countries)
9.2 Complicated UTI
- Longer duration (7–14 days) of antibiotics based on culture:
- Fluoroquinolones (e.g., ciprofloxacin)
- Ceftriaxone
- Piperacillin-tazobactam (for severe cases)
9.3 Pyelonephritis
- Initial IV therapy (ceftriaxone, aminoglycosides), followed by oral antibiotics based on culture for 10–14 days.
9.4 Recurrent UTI
- Post-coital prophylaxis
- Continuous low-dose prophylaxis (e.g., nitrofurantoin)
- Vaginal estrogen cream for postmenopausal women
9.5 Catheter-Associated UTIs (CAUTI)
- Remove or replace catheter
- Culture-directed antibiotics
10. Prevention Strategies
- Adequate hydration
- Urinating after sexual intercourse
- Avoiding irritating feminine products
- Good perineal hygiene (wiping front to back)
- Limiting use of spermicides
- Regular catheter care in hospital settings
- Screening and treating asymptomatic bacteriuria in pregnancy
11. Complications of Untreated UTIs
- Pyelonephritis
- Renal abscess
- Urosepsis
- Kidney scarring (especially in children)
- Chronic kidney disease
- Preterm labor or low birth weight (in pregnancy)
- Urethral stricture (in recurrent or neglected cases)
Conclusion
Urinary Tract Infections are highly prevalent and often recurrent, posing a notable burden on both individual health and public healthcare systems. Though usually treatable, the increasing incidence of antimicrobial resistance, particularly in recurrent or catheter-associated UTIs, is alarming. Early diagnosis, appropriate antibiotic use, patient education, and targeted prevention strategies remain the cornerstone of effective UTI management. A multidimensional approach encompassing microbiological insight, clinical vigilance, and public health policies is essential to curb the global impact of UTIs.

