The World Health Organization (WHO) has recently unveiled a comprehensive strategic framework aimed at enhancing the prevention and control of Mpox (Monkeypox). This framework marks a significant step in global health efforts to combat the resurgence and spread of this zoonotic viral disease, which has seen an uptick in cases in various regions worldwide.
Understanding Mpox
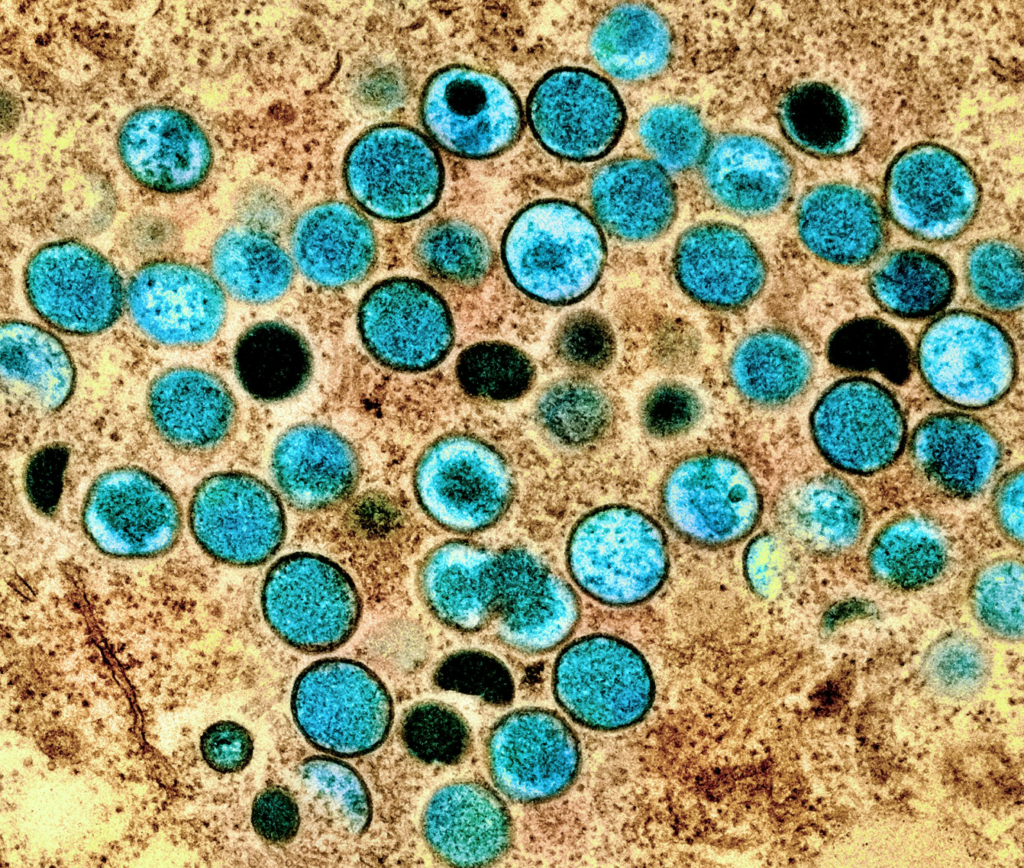
Mpox, also known as Monkeypox, is a viral disease caused by the monkeypox virus, which belongs to the Orthopoxvirus genus in the family Poxviridae. The disease is similar to smallpox but generally less severe. It was first identified in laboratory monkeys in 1958, with the first human case reported in 1970 in the Democratic Republic of the Congo. Mpox primarily occurs in central and western African countries, often in proximity to tropical rainforests, but has increasingly been reported in non-endemic countries due to international travel and trade.
Current Challenges
The resurgence of Mpox cases globally poses several challenges:
Epidemiological Surveillance: Inconsistent and insufficient surveillance systems make it difficult to track the spread of the disease.
Healthcare Infrastructure: Limited resources and healthcare infrastructure in endemic regions hinder effective response measures.
Public Awareness: Lack of awareness and misinformation about the disease contribute to its spread and hinder prevention efforts.
Animal-to-Human Transmission: Continued interaction between humans and wildlife reservoirs increases the risk of transmission.
Key Components of the Strategic Framework:
The WHO’s strategic framework for Mpox prevention and control is structured around five key components:
1. Strengthening Surveillance and Laboratory Capacity
Enhanced Monitoring: Implementing robust surveillance systems to monitor and report Mpox cases promptly.
Laboratory Networks: Establishing and strengthening laboratory networks for accurate and timely diagnosis of Mpox.
Data Sharing: Promoting the sharing of epidemiological data among countries and relevant health organizations to track and respond to outbreaks effectively.
2. Improving Preparedness and Response
Rapid Response Teams: Forming and training rapid response teams to handle outbreaks efficiently.
Emergency Preparedness Plans: Developing and updating national and regional emergency preparedness plans specific to Mpox.
Simulation Exercises: Conducting regular simulation exercises to test and improve response strategies.
3. Enhancing Public Awareness and Risk Communication
Public Education Campaigns: Launching public education campaigns to inform communities about Mpox symptoms, transmission, and prevention.
Community Engagement: Engaging with community leaders and local organizations to disseminate accurate information and counteract misinformation.
Media Collaboration: Collaborating with media outlets to ensure widespread and accurate reporting on Mpox.
4. Strengthening Healthcare Systems
Capacity Building: Training healthcare workers in Mpox detection, treatment, and prevention measures.
Resource Allocation: Ensuring adequate allocation of medical resources, including personal protective equipment (PPE), vaccines, and antiviral drugs.
Infection Control: Implementing stringent infection control protocols in healthcare facilities to prevent nosocomial transmission.
5. Promoting Research and Development
Vaccine Development: Supporting research into effective vaccines and treatments for Mpox.
Epidemiological Studies: Conducting epidemiological studies to understand the transmission dynamics and risk factors associated with Mpox.
Innovative Technologies: Exploring innovative technologies, such as digital health tools and mobile applications, to enhance disease surveillance and response efforts.
Conclusion:
The WHO’s strategic framework for Mpox prevention and control represents a holistic and proactive approach to tackling the disease. By strengthening surveillance, improving preparedness, enhancing public awareness, bolstering healthcare systems, and promoting research, the framework aims to mitigate the impact of Mpox and prevent future outbreaks.
Collaboration among countries, health organizations, and communities will be crucial for the successful implementation of this framework. As we move forward, continued vigilance and coordinated efforts will be essential in safeguarding public health and ensuring a swift and effective response to Mpox outbreaks.
For more detailed information on the WHO’s strategic framework for Mpox, you can visit the official WHO website or access the full report https://www.who.int

